preventing Devastating Strokes: Understanding and Managing Anticoagulants
Table of Contents
- 1. preventing Devastating Strokes: Understanding and Managing Anticoagulants
- 2. What CHA₂DS₂-VASc score in women strongly indicates a need for oral anticoagulation?
- 3. Optimizing Anticoagulation: A Practical Guide for Primary Care Physicians Prescribing Blood Thinners in Atrial Fibrillation
- 4. Assessing Stroke Risk: the CHA₂DS₂-vasc Score
- 5. Choosing the Right anticoagulant: NOACs vs. Warfarin
- 6. Practical Tips for NOAC Prescribing
- 7. Managing Bleeding Events: A Step-by-Step Approach
For individuals at risk of serious medical events like stroke and pulmonary embolism, anticoagulants are a vital class of medications. Cardiologist Dr. Benitez explains how these drugs work and what patients need to know for their safe and effective use.
The Threat of Blood Clots
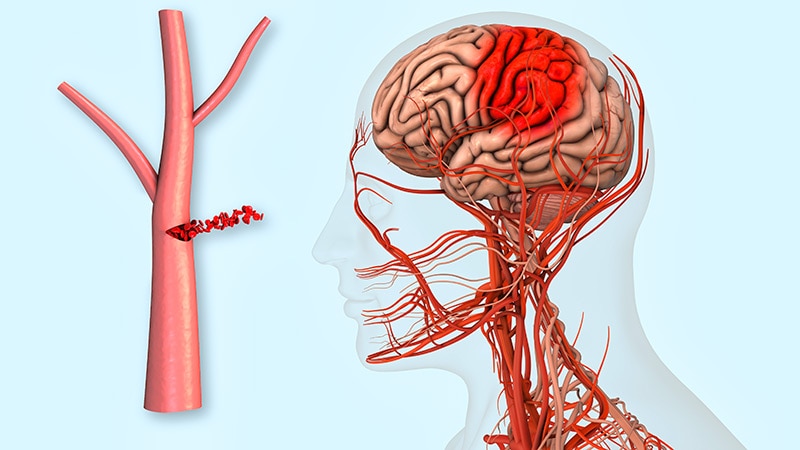
Blood clots, also known as thrombi, can form in various parts of the body and pose notable health risks. One common concern,especially for individuals with atrial fibrillation,is the formation of clots within the heart’s upper chambers. As Dr. Benitez explains, “If a clot… were to break lose from the inside of the top chamber and be pumped with the blood to the brain, it could cause a major stroke.”
Stroke is a life-altering event, frequently enough leaving survivors with permanent and significant disability. Anticoagulants play a crucial role in mitigating this risk. “The oral anticoagulant greatly reduces the risk of the formation of these blood clots and subsequent stroke,” Dr. Benitez states. “In the setting of atrial fibrillation, anticoagulation greatly reduces the patient’s risk of stroke.”
Another dangerous scenario involves blood clots forming in the leg veins,a condition known as deep venous thrombosis (DVT). If such a clot detaches, it can travel to the lungs via the heart, causing a pulmonary embolism. “This event, pulmonary embolism, can cause critical illness or even death; the risk can be greatly reduced through the use of oral anticoagulants,” Dr.Benitez emphasizes.
Key Principles for Anticoagulant Use
For these medications to be effective, adherence to prescribed regimens is paramount. Dr. Benitez stresses the importance of daily use for newer direct oral anticoagulants (DOACs) like apixaban and rivaroxaban. “In the case of the new direct oral anticoagulants, such as apixaban or rivaroxaban, the drugs both work very quickly but also wear off very quickly,” he explains. “This means that even missing just 2-3 days is enough for the blood to again clot normally.It is essential that the drugs be taken daily to prevent stroke.”
While warfarin, an older anticoagulant, has a more prolonged effect, and missing a single dose may not instantly impact anticoagulation levels, consistent daily intake remains the best practice. “While missing a single dose [of warfarin] is unlikely to markedly change the degree of anticoagulation, it’s still best to remind patients not to miss doses and take this daily as prescribed,” Dr. benitez advises.
Navigating Potential Side effects and Interactions
A critical aspect of anticoagulant therapy is managing potential drug-drug interactions. When introducing new medications, including antibiotics, it’s vital to ensure they don’t interfere with the anticoagulant’s effectiveness. “It is indeed extremely critically important with warfarin – and to a lesser degree with direct oral anticoagulants – to always make certain that there is no drug-drug interaction that might affect the degree of anticoagulation when new medications are introduced,” Dr. Benitez cautions.
Patients may experience minor bleeding, such as gum bleeding during dental flossing or occasional nosebleeds. These typically resolve on their own and don’t require immediate medical intervention. Though, self-monitoring and knowing when to seek help is critically important. “If bleeding will not readily stop then medical attention is needed,” Dr. Benitez states. “Patients who incur major injury or trauma are likely to be taken to an emergency facility where it is important for the staff caring for them to know what anticoagulant they are taking, the dose, and when they last took it.” He also notes the availability of “reversal agents… to normalize blood clotting.”
Dietary Considerations, Especially with Warfarin
Unlike many medications, anticoagulants generally do not have significant food interactions or require strict dietary restrictions. However, a notable exception exists for warfarin users. Warfarin is a vitamin K antagonist, and vitamin K essentially acts as an antidote. “With warfarin… it is indeed essential that the patient limit their intake of food containing vitamin K, as it is essentially an antidote or reversal agent for the anticoagulant,” Dr. Benitez explains.
While leafy green vegetables like spinach and kale are well-known sources of vitamin K, Dr. Benitez points out that other foods can also be rich in this vitamin. These include cauliflower and various soy products.”It is indeed critically important for the patient to familiarize themselves with vitamin K-containing foods and to keep the intake of them low and steady from day to day if they are taking warfarin,” he advises. Maintaining a consistent intake of vitamin K-rich foods, rather than drastically changing consumption, is key for patients on warfarin.
by understanding how anticoagulants work, adhering to prescribed regimens, and being aware of potential interactions and dietary considerations, patients can significantly reduce their risk of debilitating strokes and other serious thromboembolic events. Open communication with healthcare providers is essential for effective and safe management of these life-saving medications.
What CHA₂DS₂-VASc score in women strongly indicates a need for oral anticoagulation?
Optimizing Anticoagulation: A Practical Guide for Primary Care Physicians Prescribing Blood Thinners in Atrial Fibrillation
Assessing Stroke Risk: the CHA₂DS₂-vasc Score
Accurate stroke risk stratification is the cornerstone of appropriate anticoagulation in atrial fibrillation (AFib). The CHA₂DS₂-VASc score remains the gold standard. Remember, this isn’t just about ticking boxes; itS a clinical judgment.
Congestive heart failure (1 point)
Hypertension (1 point)
A₂ge ≥75 years (2 points)
Diabetes mellitus (1 point)
S₂troke/TIA/thromboembolism history (2 points)
Vascular disease (1 point) – peripheral artery disease, coronary artery disease, etc.
Age 65-74 years (1 point)
Sex category – female (1 point)
A score of 0 in men or 1 in women generally doesn’t warrant anticoagulation, but consider individual patient factors. Scores ≥1 in men and ≥2 in women strongly indicate a need for oral anticoagulation. Don’t forget to reassess the score periodically, as a patient’s clinical picture can change. Stroke prevention in atrial fibrillation is the primary goal.
Choosing the Right anticoagulant: NOACs vs. Warfarin
The landscape of anticoagulation therapy has evolved considerably. While warfarin remains an option, Non-Vitamin K Oral Anticoagulants (NOACs) – including dabigatran, rivaroxaban, apixaban, and edoxaban – are frequently enough preferred due to their more predictable pharmacokinetics and reduced monitoring requirements.
Here’s a rapid comparison:
| Feature | Warfarin | NOACs |
|——————-|—————————————-|—————————————-|
| Monitoring | Frequent INR checks | Generally no routine monitoring |
| Food Interactions| Important | Fewer |
| Drug Interactions| Numerous | Moderate |
| Bleeding Risk | Higher, influenced by INR variability | Generally lower, more predictable |
| Reversal Agent | Vitamin K | Idarucizumab (dabigatran), andexanet alfa (rivaroxaban, apixaban) |
consider patient-specific factors when choosing:
Kidney Function: NOAC dosing adjustments are crucial in renal impairment. Apixaban generally has the least renal impact.
Bleeding Risk: Assess using tools like HAS-BLED (Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly, Drugs/alcohol).
Patient Preference: Discuss the pros and cons of each option with the patient, considering their lifestyle and adherence potential.Oral anticoagulants require consistent use.
Practical Tips for NOAC Prescribing
Dosing: Pay close attention to dosing guidelines based on creatinine clearance. Utilize online dosing calculators (available from the manufacturers) to ensure accuracy.
Adherence: Emphasize the importance of taking the medication exactly as prescribed. Missed doses can significantly increase stroke risk.
Drug Interactions: Be vigilant about potential drug interactions,especially with strong P-glycoprotein inhibitors or inducers.
Peri-Procedural Management: Develop a clear plan for managing anticoagulation around surgical or invasive procedures. Guidelines vary depending on the NOAC and the procedure’s bleeding risk.
Patient Education: Provide clear, written instructions on medication use, potential side effects, and emergency contact data.
Managing Bleeding Events: A Step-by-Step Approach
Even with NOACs,bleeding can occur. A systematic approach is essential.
- Assess Severity: determine the extent of bleeding (minor vs.major).
- Stop the Anticoagulant: Immediately discontinue the NOAC.
- Supportive Care: Provide appropriate supportive care (e.g., fluid resuscitation, blood transfusions).
- Consider Reversal Agents:
*Dabigat