Intravenous Iron Therapy Shows Significant Benefits for Heart Failure patients with Iron deficiency
Table of Contents
- 1. Intravenous Iron Therapy Shows Significant Benefits for Heart Failure patients with Iron deficiency
- 2. What is iron deficiency without anemia (IDNA) and why is it often overlooked in heart failure patients?
- 3. Intravenous Iron Improves Cardiovascular Outcomes in Heart Failure Patients
- 4. The Link Between Iron Deficiency and Heart Failure
- 5. How Intravenous Iron Impacts Heart Failure
- 6. Understanding the Mechanisms of Action
- 7. Identifying Iron Deficiency in Heart Failure Patients
- 8. IV Iron Formulations: What are the Options?
- 9. Safety Considerations and Potential Side Effects
- 10. Real-World Example: The IRON-HF Trial
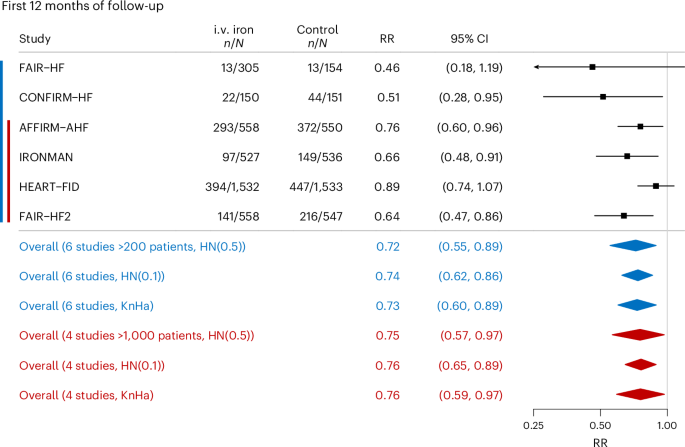
A extensive systematic review and meta-analysis has revealed that intravenous iron therapy offers substantial advantages for individuals diagnosed with heart failure who also experience iron deficiency. The groundbreaking findings, published in the esteemed journal Nature Medicine, underscore the critical role of iron repletion in managing this prevalent and often debilitating condition.
The study, led by S. D. Anker and colleagues, meticulously examined existing research to consolidate evidence on the efficacy of this therapeutic approach. Their analysis indicates that administering iron directly into the bloodstream can lead to significant improvements in the quality of life and physical capabilities of heart failure patients.
Iron deficiency is a common comorbidity among heart failure patients, often contributing to an
What is iron deficiency without anemia (IDNA) and why is it often overlooked in heart failure patients?
Intravenous Iron Improves Cardiovascular Outcomes in Heart Failure Patients
The Link Between Iron Deficiency and Heart Failure
heart failure (HF) is a complex clinical syndrome, and increasingly, we’re recognizing the meaningful role iron deficiency (ID) plays in its progression and outcomes. It’s no longer simply about the heart’s pumping ability; addressing underlying deficiencies like iron can dramatically improve a patient’s quality of life and reduce hospitalizations. Iron is crucial for oxygen transport via hemoglobin, but also plays a vital role in cardiac muscle function, energy production within heart cells (mitochondrial function), and overall cardiovascular health.
many heart failure patients, even without anemia, exhibit ID – a condition known as iron deficiency without anemia (IDNA). This is especially common in those with chronic heart failure, and it’s often overlooked.Traditional markers like serum ferritin can be misleading, as they are frequently enough elevated due to inflammation, masking the true iron status.
How Intravenous Iron Impacts Heart Failure
Intravenous (IV) iron therapy is gaining prominence as a key component of heart failure management.Unlike oral iron supplements, IV iron bypasses the gut, leading to faster and more complete iron repletion. This is critical for patients with HF, who often have impaired gut absorption. Here’s how IV iron demonstrably improves cardiovascular outcomes:
Improved Exercise Capacity: Studies consistently show that IV iron significantly increases exercise tolerance in HF patients. This translates to a greater ability to perform daily activities and a better overall quality of life.
Reduced Hospitalizations: A major benefit of IV iron is a reduction in heart failure-related hospitalizations. By addressing the underlying iron deficiency,the heart functions more efficiently,lessening the burden on the cardiovascular system.
Enhanced quality of Life: Patients report feeling less fatigued, more energetic, and generally healthier after IV iron treatment. This improvement in well-being is a significant outcome.
Potential for Reduced Mortality: While more research is ongoing, emerging evidence suggests that IV iron may even contribute to reduced mortality rates in select heart failure populations.
Understanding the Mechanisms of Action
The benefits of IV iron extend beyond simply increasing hemoglobin levels. Several key mechanisms are at play:
Enhanced mitochondrial Function: Iron is a critical component of enzymes involved in mitochondrial respiration. Replenishing iron stores improves mitochondrial function, boosting energy production within heart muscle cells.
Improved cardiac Contractility: Adequate iron levels support optimal cardiac muscle contraction, leading to a stronger and more efficient heartbeat.
Reduced Inflammation: Iron deficiency can exacerbate inflammation, which contributes to HF progression. IV iron can help modulate the inflammatory response.
Increased VO2 Max: IV iron has been shown to increase maximal oxygen uptake (VO2 max), a key indicator of cardiovascular fitness.
Identifying Iron Deficiency in Heart Failure Patients
Accurate diagnosis is paramount. Relying solely on hemoglobin levels is insufficient. A extensive iron assessment should include:
- Serum Ferritin: While not always reliable due to inflammation, it’s a starting point.
- Transferrin Saturation (TSAT): Measures the percentage of transferrin that is bound to iron.A low TSAT (<20-30%) suggests ID.
- Serum Iron: Measures the amount of iron circulating in the blood.
- total Iron Binding Capacity (TIBC): Measures the blood’s capacity to bind iron.
- C-Reactive Protein (CRP): To assess inflammation levels, which can affect ferritin interpretation.
- Hepcidin: A hormone that regulates iron absorption and release. Elevated hepcidin levels can indicate inflammation-induced iron restriction. (Though not widely available yet, it’s becoming increasingly vital).
IV Iron Formulations: What are the Options?
Several IV iron formulations are available, each with its own characteristics:
Iron Dextran: An older formulation, associated with a higher risk of allergic reactions.
Iron Sucrose: Generally well-tolerated, but requires slower infusion rates.
Ferric Gluconate: Another commonly used option with a good safety profile.
Ferumoxytol: A newer formulation with a higher single-dose capacity, potentially reducing the number of infusions needed.
Iron Isomaltoside 1000: Offers a high single-dose capacity and a favorable safety profile.
The choice of formulation depends on individual patient factors, including allergy history, renal function, and the severity of iron deficiency.
Safety Considerations and Potential Side Effects
while generally safe,IV iron therapy can have side effects. these can range from mild infusion reactions (e.g., flushing, nausea) to more serious allergic reactions.
Hypotension: A drop in blood pressure can occur during or after infusion.
Allergic Reactions: Monitor patients closely for signs of anaphylaxis.
Iron Overload: Rare,but possible with excessive dosing.
Joint Pain: Some patients experience transient joint pain after IV iron.
careful patient selection, appropriate dosing, and close monitoring during and after infusion are crucial to minimize risks.
Real-World Example: The IRON-HF Trial
The IRON-HF trial, published in The Lancet* in 2022, provided compelling evidence for the benefits of IV iron in heart failure patients. This randomized, controlled trial demonstrated that IV ferric