Discover the latest in health: evidence‑based wellness tips, medical breakthroughs, nutrition guidance, fitness insights, and expert advice for a healthier, happier life.
The Silent Spread: How Bacteria Trade Antibiotic Resistance
Table of Contents
- 1. The Silent Spread: How Bacteria Trade Antibiotic Resistance
- 2. the Rise of Superbugs and a looming Crisis
- 3. Unlocking the Secrets of Resistance
- 4. Plasmids: the Genetic Exchange Network
- 5. Where Bacteria Swap Genes
- 6. The Danger of Combined Traits
- 7. New Strategies to Disrupt Resistance
- 8. the Evolution of “Super Plasmids”
- 9. From Spinach to Sepsis: A New Frontier
- 10. Understanding Antibiotic Resistance: A Long-Term Perspective
- 11. Frequently Asked Questions About Antibiotic Resistance
- 12. How do mobile genetic elements contribute to the spread of antibiotic resistance genes between different bacterial species?
- 13. Unveiling Molecular Mechanisms: how UCSC-led Global Research Clarifies Antibiotic Resistance in Bacteria
- 14. The Growing Threat of Antimicrobial Resistance (AMR)
- 15. UCSC Research: A Deep Dive into Resistance Genes
- 16. Key Findings from the UCSC Study:
- 17. Mechanisms of Antibiotic Resistance: A Closer Look
- 18. The Role of the Microbiome in AMR
- 19. Combating Antibiotic Resistance: Strategies and Innovations
- 20. Real-World Example: Carbapenem-Resistant Enterobacteriaceae (CRE)
A recent outbreak linked to contaminated food last fall, affecting over 100 individuals across 14 states, highlighted the growing threat of antibiotic-resistant bacteria. The Centers for Disease Control and Prevention pinpointed the source to Escherichia coli found on raw onions served at a major fast-food chain. This incident underscores a critical battle against microorganisms that are rapidly evolving to resist conventional treatments.
the Rise of Superbugs and a looming Crisis
While moast of the over 700 varieties of E. coli are benign, certain strains pose significant health risks and demand antibiotic intervention. Though, bacteria are adept at developing resistance mechanisms, whether by dismantling the medication or building defenses against it.Alarmingly, the pace of antibiotic resistance is outpacing the progress of new drugs, prompting the World Health Institution to label this phenomenon a major global health emergency.
Unlocking the Secrets of Resistance
Researchers are pivoting away from solely searching for new drugs and focusing on understanding the fundamental origins of antibiotic resistance in bacteria. Scientists at the University of California, Santa Cruz, are investigating how bacteria acquire the ability to neutralize drugs, primarily through specific genes. These genes aren’t created in isolation; they are frequently enough transferred between bacterial cells.
Plasmids: the Genetic Exchange Network
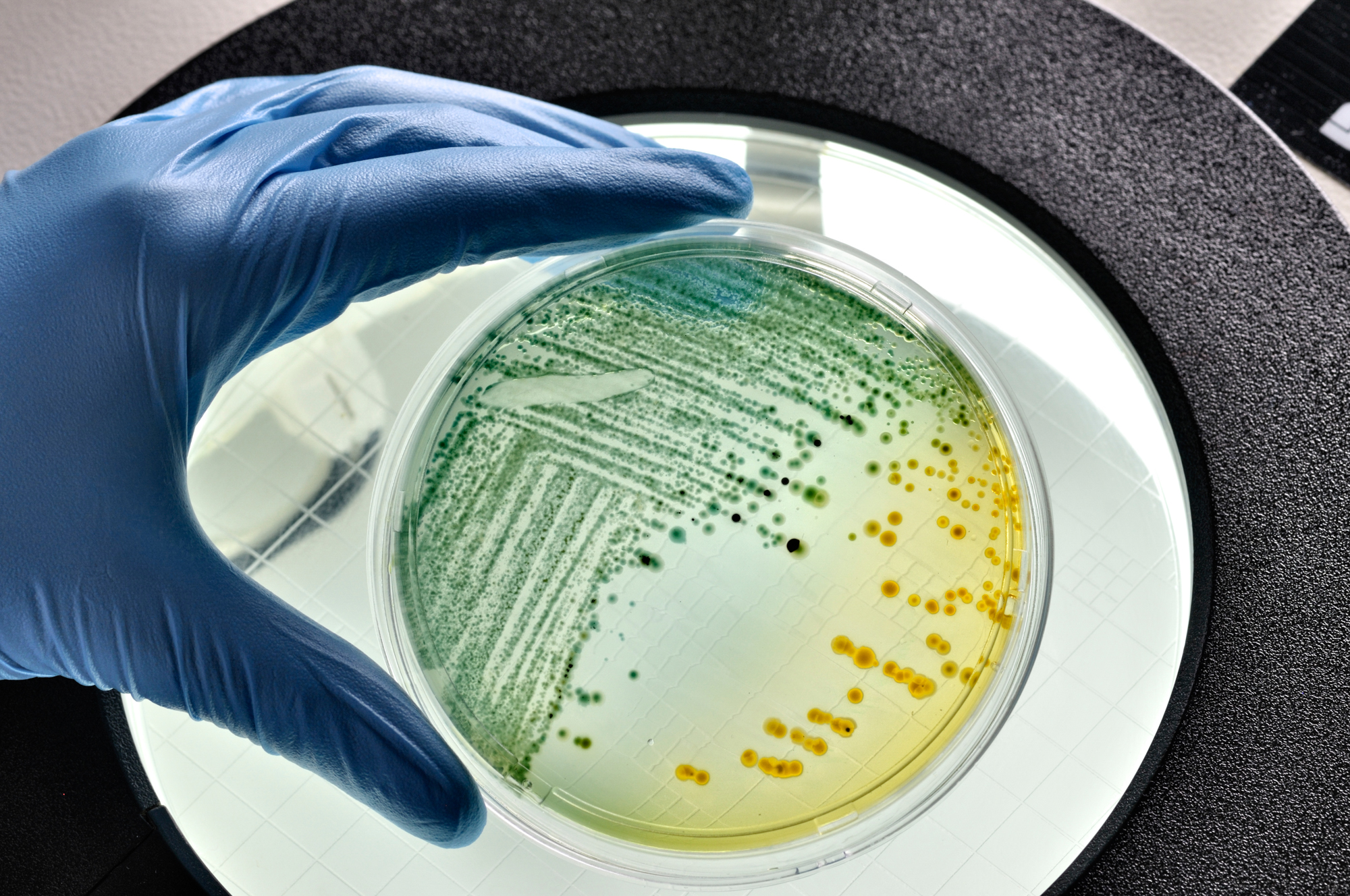
Antibiotic-resistant genes frequently reside on plasmids-small, circular DNA structures separate from the main bacterial genome. these plasmids act as mobile genetic elements,facilitating rapid gene transfer between bacteria,much like “booster packs” of genetic information. In 2022, a study revealed how these resistance genes readily jump between bacterial species in various settings, including food and clinical environments.
The primary method of this transfer is conjugation, where bacteria form a direct connection to exchange DNA. Plasmids contain the genetic instructions for this process, effectively ensuring their survival and propagation of resistance. “Plasmids are known as selfish genetic elements,” explains a leading researcher. “They prioritize their own perpetuation, regardless of the host.”

Where Bacteria Swap Genes
Genetic exchange is most common in environments where diverse bacterial strains converge, such as wastewater treatment facilities. However, bacteria can also share plasmids within the human body, meaning a strain initially from the environment can gain resistance genes and spread them amongst human populations.
The Danger of Combined Traits
Crucially,plasmids frequently enough carry both antibiotic resistance and virulence genes-genes that enhance a bacterium’s ability to cause disease. This combination can transform a harmless bacterium into a hazardous pathogen. While plasmids benefit bacterial survival, they also demand energy from the host. When a plasmid no longer provides an advantage, bacteria may discard it to free up resources.
New Strategies to Disrupt Resistance
Scientists are exploring this “plasmid loss” phenomenon as a potential therapeutic strategy.Researchers are currently screening compounds to identify substances that encourage bacteria to eject plasmids or create stress that forces them to relinquish these genetic elements. The aim is to eliminate the genes responsible for drug resistance.
the Evolution of “Super Plasmids”
Plasmids can accumulate multiple resistance genes over time, resulting in “super plasmids” resistant to a wide range of antibiotics. This process, termed “genetic capitalism,” leads to increasingly complex infections that are difficult to treat. Methicillin-resistant Staphylococcus aureus (MRSA) serves as a prime example.
According to the CDC, drug-resistant infections caused 1.27 million deaths globally in 2019. Moreover, the six most common types of resistant infections increased by 20% in the United States during the COVID-19 pandemic, suggesting a worsening crisis.
From Spinach to Sepsis: A New Frontier
Researchers recently identified a dangerous strain of E. coli in spinach sold in Mexico. this strain,capable of causing both intestinal and urinary tract infections,highlights a new concern: the contamination of agricultural products. Inquiry suggests the spinach may have been irrigated with insufficiently treated wastewater, allowing the bacteria to thrive.
| Type of E. coli | Infection Type | Resistance Pattern |
|---|---|---|
| InPEC | Intestinal Infections | Variable |
| ExPEC | Urinary Tract Infections, Meningitis | Increasingly Antibiotic-Resistant |
Understanding Antibiotic Resistance: A Long-Term Perspective
Antibiotic resistance is not a new problem, but it is an escalating one. The overuse and misuse of antibiotics in human medicine and agriculture are major drivers of this trend.Prudent antibiotic use, improved hygiene practices, and continued research are vital for safeguarding the effectiveness of these life-saving drugs.
Did You Know? The CDC estimates that at least 30% of antibiotics prescribed in the U.S. are unnecessary.
Pro Tip: Always complete the full course of antibiotics as prescribed by your doctor, even if you start feeling better.
Frequently Asked Questions About Antibiotic Resistance
- What is antibiotic resistance? It occurs when bacteria evolve to survive exposure to antibiotics,rendering the drugs ineffective.
- How do bacteria become resistant to antibiotics? Through genetic mutations and the transfer of resistance genes, frequently enough via plasmids.
- What are plasmids? Small,circular DNA molecules that can carry genes conferring antibiotic resistance.
- Can antibiotic resistance spread between people? Yes, it can spread through direct contact, contaminated surfaces, and the food supply.
- What can be done to combat antibiotic resistance? Reduce unnecessary antibiotic use, improve infection control, and develop new drugs and therapies.
- is antibiotic resistance a global threat? Absolutely, the World Health Organization recognizes it as one of the biggest health challenges facing humanity.
- How does food contamination contribute to antibiotic resistance? Contaminated food can spread resistant bacteria, leading to infections in humans.
What role do you think individual choices play in the broader issue of antibiotic resistance? Share your thoughts in the comments below!
Are you concerned about the presence of antibiotic-resistant bacteria in the food supply? Let us know your perspective.
How do mobile genetic elements contribute to the spread of antibiotic resistance genes between different bacterial species?
Unveiling Molecular Mechanisms: how UCSC-led Global Research Clarifies Antibiotic Resistance in Bacteria
The Growing Threat of Antimicrobial Resistance (AMR)
Antibiotic resistance, often termed antimicrobial resistance, is a critical global health challenge. Bacteria, viruses, fungi, and parasites are evolving resistance to the medicines designed to kill them, making infections harder to treat and increasing the risk of disease spread. This isn’t just a future problem; it’s happening now. The World Health Association (WHO) considers AMR one of the top 10 global public health threats facing humanity. Understanding the molecular basis of antibiotic resistance is paramount to developing effective countermeasures.
UCSC Research: A Deep Dive into Resistance Genes
Recent, groundbreaking research led by the University of California, Santa Cruz (UCSC) has significantly advanced our understanding of how bacteria develop and spread antibiotic resistance genes. This international collaborative effort, involving researchers from multiple continents, focused on identifying the specific genetic mechanisms driving resistance to several key classes of antibiotics.
The UCSC team employed advanced genomic sequencing and bioinformatics techniques to analyze thousands of bacterial genomes. Their findings pinpointed several previously unknown resistance determinants and elucidated the pathways through which thes genes are transferred between bacteria – a process known as horizontal gene transfer.
Key Findings from the UCSC Study:
* Mobile Genetic Elements: The research highlighted the crucial role of mobile genetic elements (MGEs) – such as plasmids, transposons, and integrons – in disseminating resistance genes. These elements act like “vehicles” carrying resistance genes across bacterial species, even those distantly related.
* Novel Resistance Genes: The study identified several novel genes conferring resistance to carbapenems,a class of “last-resort” antibiotics. This revelation is notably alarming,as carbapenem resistance is rapidly increasing globally.
* mutations and Gene Amplification: Beyond gene transfer, the research also revealed specific mutations within bacterial genes that contribute to reduced antibiotic susceptibility. Gene amplification, where bacteria increase the number of copies of a particular gene, was also observed as a resistance mechanism.
* Biofilm Formation & Resistance: The study confirmed a strong correlation between biofilm formation and increased antibiotic resistance. Biofilms, communities of bacteria encased in a protective matrix, hinder antibiotic penetration and promote gene transfer.
Mechanisms of Antibiotic Resistance: A Closer Look
Understanding how bacteria resist antibiotics is crucial for developing new strategies. Here’s a breakdown of the major mechanisms:
- Enzymatic Degradation: Bacteria produce enzymes that break down the antibiotic molecule, rendering it ineffective. Beta-lactamases,for example,degrade penicillin and other beta-lactam antibiotics.
- Target Modification: Mutations in the bacterial target site (e.g., ribosomes, cell wall synthesis enzymes) alter its structure, preventing the antibiotic from binding effectively.
- Efflux Pumps: Bacteria utilize efflux pumps to actively transport antibiotics out of the cell,reducing their intracellular concentration.
- Reduced Permeability: Changes in the bacterial cell wall or membrane can reduce the entry of antibiotics into the cell.
- Bypass Pathways: Bacteria develop alternative metabolic pathways that circumvent the antibiotic’s target.
The Role of the Microbiome in AMR
The human gut microbiome – the community of microorganisms living in our digestive tract – plays a significant role in the advancement and spread of antibiotic resistance.
* Reservoir of Resistance Genes: The microbiome serves as a vast reservoir of resistance genes. Antibiotic use, even in agriculture, can select for resistant bacteria in the gut, which can then transfer these genes to pathogenic bacteria.
* Microbiome Disruption: Antibiotics disrupt the balance of the microbiome, creating opportunities for resistant bacteria to colonize and proliferate.
* fecal-Oral Transmission: Resistant bacteria can be transmitted through the fecal-oral route, contributing to the spread of AMR in the community.
Combating Antibiotic Resistance: Strategies and Innovations
Addressing AMR requires a multifaceted approach. Here are some key strategies:
* Antibiotic Stewardship: Implementing programs to optimize antibiotic use in healthcare and agriculture, reducing unnecessary prescriptions and promoting appropriate dosing.
* New Antibiotic Development: Investing in research and development of novel antibiotics with new mechanisms of action. This is a significant challenge, as the economic incentives for antibiotic development are often limited.
* Alternative Therapies: Exploring alternative therapies, such as phage therapy (using viruses to kill bacteria), antimicrobial peptides, and immunotherapy.
* Diagnostics: Developing rapid and accurate diagnostic tests to identify infections and determine antibiotic susceptibility, enabling targeted treatment. rapid diagnostics are crucial for reducing inappropriate antibiotic use.
* Infection Prevention and Control: Strengthening infection prevention and control measures in healthcare settings to prevent the spread of resistant bacteria.
* Global Surveillance: Enhancing global surveillance of AMR to track the emergence and spread of resistance patterns.
Real-World Example: Carbapenem-Resistant Enterobacteriaceae (CRE)
Carbapenem-resistant Enterobacteriaceae (CRE) are a particularly concerning group of bacteria. These bacteria are resistant to carbapenems, often the