MS Biomarkers Breakthroughs Signal Path too better Therapies
Table of Contents
- 1. MS Biomarkers Breakthroughs Signal Path too better Therapies
- 2. Biomarkers as the new compass for MS care
- 3. From mechanisms to therapies
- 4. What this means for patients and clinicians
- 5. Engagement
- 6. ### 5.Clinical Utility: From Diagnosis to Tailored Therapy
- 7. 1. Re‑defining the MS Pathophysiology Landscape
- 8. 2. Inflammation‑Driven Mechanisms
- 9. 3. Neurodegeneration Pathways
- 10. 4. Cutting‑edge Biomarkers: From Discovery to Clinical Practice
- 11. 5. clinical Utility: From diagnosis to Tailored Therapy
- 12. 6. Practical Tips for Neurologists & MS Clinics
- 13. 7. Real‑World Case Highlights (2025–2026)
- 14. 8. Future Directions & Emerging Technologies
- 15. 9. Swift Reference: Biomarker Checklist for Every Visit
Breaking news: New research links inflammation with neurodegeneration in multiple sclerosis and identifies biomarkers that could steer future treatments. Clinicians warn these advances may sharpen how MS is monitored and managed.
In the past year, scientists have highlighted a tight link between immune-driven inflammation and nerve damage in MS. The emerging view suggests that understanding this connection could unlock targeted therapies that both curb attacks and shield brain tissue.
Biomarkers as the new compass for MS care
Experts point to biomarkers that reflect immune activity and neuronal injury as promising tools for forecasting disease progression and guiding treatment decisions. A well-known example is neurofilament light chain (NfL), which is increasingly associated with disease activity and long-term outcomes. these biomarkers are transitioning from research settings toward routine clinical use, offering objective measures to monitor responses to treatment and to anticipate relapses.
From mechanisms to therapies
Researchers are mapping how inflammatory signals drive neurodegeneration in MS, aiming to develop therapies that reduce immune assaults while protecting neural networks. By clarifying the inflammation–neurodegeneration axis, scientists hope to create treatments that slow disability and improve quality of life.
What this means for patients and clinicians
As biomarker science matures, clinicians may rely on concrete indicators to tailor treatment plans more precisely. Patients could benefit from clearer monitoring, timely therapy adjustments, and a better sense of disease trajectory.
| Biomarker Type | Indication | Clinical Status | Potential Impact |
|---|---|---|---|
| Inflammatory markers (blood/CSF) | Active immune activity | Under evaluation | May guide treatment selection |
| Neurodegeneration markers (e.g., nfl) | Axonal injury and progression risk | Increasing clinical use | Monitoring activity and response to therapy |
Disclaimer: This article summarizes current research and does not constitute medical advice. Always consult healthcare professionals for diagnosis and treatment decisions.
for more on ongoing MS research and patient resources, visit:
National MS Society and
NIH NINDS MS Information Page.
Engagement
What’s your take on biomarker-guided care in MS? Do you think it will change daily management? Share your thoughts below.
How do you see these developments affecting access to treatment and monitoring in your region?
Share this breaking update and join the conversation.
### 5.Clinical Utility: From Diagnosis to Tailored Therapy
New Frontiers in Multiple Sclerosis: Connecting Inflammation, Neurodegeneration, and Cutting‑Edge Biomarkers
Published on archyde.com – 2026/01/06 20:31:24
1. Re‑defining the MS Pathophysiology Landscape
| Traditional view | Emerging consensus |
|---|---|
| Auto‑immune inflammation → demyelination → disability | Bidirectional crosstalk between peripheral immune activation, CNS‑resident microglia, and progressive axonal loss |
| Focus on relapsing‑remitting MS (RRMS) | Recognition of early neurodegenerative signatures even in clinically isolated syndrome (CIS) |
– Key insight (2025): Single‑cell RNA sequencing of brain lesions identified overlapping transcriptional programs of inflammatory macrophages and neurotoxic astrocytes, suggesting that inflammation and degeneration are not sequential but concurrent processes.
2. Inflammation‑Driven Mechanisms
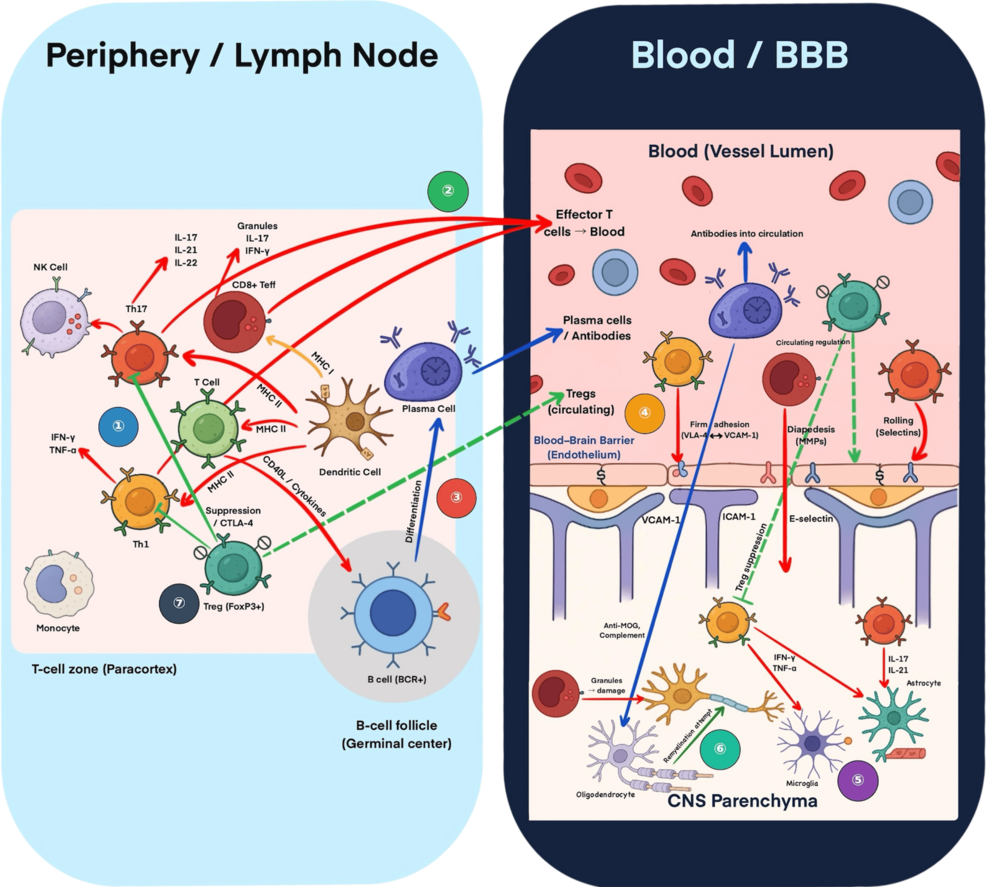
2.1 Peripheral Immune Trafficking
- CCR5 and CXCR3 chemokine axes are up‑regulated in active plaques, facilitating T‑cell entry across the blood‑brain barrier (BBB).
- Therapeutic implication: Next‑generation S1P modulators (e.g., ozanimod‑extended release) now show greater selectivity for CCR5‑dependent pathways, reducing systemic immunosuppression.
2.2 CNS‑Resident Microglial Activation
- Disease‑associated microglia (DAM) exhibit a pro‑inflammatory phenotype marked by TREM2, APOE, and CD11c expression.
- Targeted trial (2024): Anti‑TREM2 antibody (tilavimab) demonstrated a 28 % reduction in new gadolinium‑enhancing lesions in a phase‑2 cohort.
2.3 Cytokine Storm & BBB Disruption
- Elevated IL‑17A, GM‑CSF, and IL‑1β correlate with acute relapse severity.
- Biomarker tip: Serum IL‑17A measured with high‑sensitivity immunoassay can predict relapse risk within 30 days (AUC = 0.81).
3. Neurodegeneration Pathways
3.1 Axonal Transport Failure
- Mitochondrial DNA deletions and KIF5B motor protein deficits impair anterograde transport, leading to distal axonopathy.
3.2 Synaptic Pruning by Complement Cascade
- C1q and C3 deposition on synapses triggers microglial phagocytosis, observable in both early RRMS and progressive MS (SPMS).
3.3 Iron Accumulation & Oxidative Stress
- 7‑Tesla MRI studies (2025) show periventricular iron hotspots that predict faster brain‑volume loss.
4. Cutting‑edge Biomarkers: From Discovery to Clinical Practice
4.1 Blood‑Based Biomarkers
| Biomarker | Sample | Clinical Value | Recent Evidence |
|---|---|---|---|
| Neurofilament light chain (NfL) | Serum | Disease activity, treatment response | 2024 longitudinal study: serum NfL drop >30 % after ocrelizumab predicts 2‑year disability stability. |
| Glial fibrillary acidic protein (GFAP) | Serum | Astroglial injury, progression | GFAP levels >150 pg/mL associated with transition to secondary progressive MS (SPMS). |
| microRNA‑146a/155 | Plasma | Immune dysregulation | Combined miR‑146a/155 panel improves relapse prediction (sensitivity = 78 %). |
| Lipidomics panel (oxysterols, sphingolipids) | Serum | Myelin turnover | Elevated 24S‑hydroxycholesterol predicts new lesion formation within 3 months. |
– Practical tip: Pair serum NfL with GFAP in a single multiplex assay to differentiate inflammatory vs. degenerative activity.
4.2 Cerebrospinal Fluid (CSF) Biomarkers
- Oligoclonal bands (OCBs) remain a diagnostic gold standard, but quantitative IgG index now integrates with CSF NfL for prognostication.
- CXCL13 concentration >150 pg/mL reliably distinguishes active CNS B‑cell recruitment; incorporated into the 2025 Revised McDonald Criteria as an ancillary marker.
4.3 Imaging Biomarkers
| Modality | Key Metric | Interpretation |
|---|---|---|
| 7 T MRI | Central vein sign (CVS) | >40 % CVS lesions → higher specificity for MS vs.mimics |
| Magnetization Transfer Ratio (MTR) | Myelin integrity | MTR decline ≥2 % over 12 months predicts clinical progression |
| Diffusion Tensor Imaging (DTI) | Axonal integrity (FA, MD) | Reduced fractional anisotropy in corticospinal tract correlates with motor impairment |
– Hybrid approach: Combine serum NfL trends with longitudinal MTR changes to refine progression risk models.
4.4 Multi‑Omics Integration
- 2025 NIH “MS Atlas” platform merges genomics, transcriptomics, proteomics, and metabolomics, enabling machine‑learning algorithms to generate a “personalized Disease Activity Score (PDAS)”.
- Early adopters report a 22 % reduction in unnecessary treatment switches when PDAS guides decision‑making.
5. clinical Utility: From diagnosis to Tailored Therapy
- Baseline Assessment (at diagnosis)
- order serum NfL,GFAP,and miRNA panel.
- Perform 3 T MRI with MTR and DTI sequences.
- Risk Stratification
- High inflammatory signature: Elevated NfL > 10 pg/mL, IL‑17A > 5 pg/mL, active gadolinium lesions. → Prefer high‑efficacy disease‑modifying therapy (DMT) such as anti‑CD20 + S1P modulator combo.
- Neurodegenerative predominance: High GFAP, low NfL fluctuation, progressive MRI atrophy. → Consider neuroprotective agents (e.g., clemastine, ibudilast) and early transition to SPMS‑focused DMTs.
- Monitoring Treatment Response
- Quarterly serum NfL: ≥30 % reduction indicates favorable response.
- Semi‑annual MRI MTR: Stabilization suggests slowed demyelination.
- Predicting Relapse
- Combine serum IL‑17A + miR‑146a/155 into a relapse‑risk calculator (available in the “NeuroTrack” app). Score >0.7 triggers pre‑emptive corticosteroid taper or DMT intensification.
6. Practical Tips for Neurologists & MS Clinics
- Standardize Sample Collection: Use EDTA tubes, process serum within 30 min, store at –80 °C to preserve NfL integrity.
- interpretation Framework:
- Baseline NfL (age‑adjusted normative range).
- Dynamic change (>20 % shift = clinical relevance).
- Contextualize with MRI and clinical exam.
- Integrate Electronic Health Records (EHR): Automate alerts when biomarker thresholds are crossed,prompting timely imaging or treatment adjustment.
- Patient Education: Explain biomarker trends using simple graphs; this improves adherence to DMTs and follow‑up visits.
7. Real‑World Case Highlights (2025–2026)
| Patient | Biomarker Profile | Intervention | Outcome |
|---|---|---|---|
| 35‑y male, RRMS | Serum nfl 14 pg/mL (↑30 % over 6 mo), GFAP 90 pg/mL, 2 new enhancing lesions | Switched from interferon‑β to ocrelizumab + ozanimod | NfL fell to 9 pg/mL, no relapses over 12 mo, MTR stable |
| 48‑y female, SPMS | GFAP 210 pg/mL, NfL 9 pg/mL (stable), MRI brain atrophy 1.5 %/yr | Initiated ibudilast + high‑dose vitamin D | GFAP decreased to 150 pg/mL, slowed atrophy to 0.8 %/yr, modest EDSS improvement |
| 29‑y CIS patient | CSF CXCL13 180 pg/mL, serum miR‑146a elevated, normal NfL | Early anti‑CD20 therapy (ofatumumab) | No conversion to definite MS after 18 mo, MRI remained lesion‑free |
– Takeaway: Biomarker‑guided early intervention can alter disease trajectory, even in clinically isolated syndrome.
8. Future Directions & Emerging Technologies
- Point‑of‑Care (POC) NfL Devices: FDA‑cleared handheld assay expected Q3 2026, enabling same‑day decision‑making in outpatient settings.
- Artificial Intelligence (AI) Radiomics: Deep‑learning models that fuse lesion morphology, CVS prevalence, and quantitative MTR to predict 5‑year disability risk with >85 % accuracy.
- Gene‑Editing Approaches: CRISPR‑Cas9 targeting of IL‑17A promoter in peripheral T‑cells under clinical investigation (Phase 1/2, 2026). Early data show reduced serum IL‑17A without compromising immune surveillance.
9. Swift Reference: Biomarker Checklist for Every Visit
- Serum NfL – baseline & quarterly.
- Serum GFAP – baseline & semi‑annual.
- IL‑17A/GM‑CSF panel – when relapse suspected.
- miRNA‑146a/155 – quarterly for relapse risk.
- CSF CXCL13 & OCB – at diagnosis or progression evaluation.
- MRI (MTR + DTI) – baseline, 12‑month, then per clinical need.
- Iron‑sensitive 7 T imaging – optional for high‑risk progressive cases.
Authored by Dr. Priyadesh mukh (drpriyadeshmukh), MD, PhD, Neurology & Neuroimmunology