Aortic Dissection Mistaken for Ileus in Case Study
Table of Contents
- 1. Aortic Dissection Mistaken for Ileus in Case Study
- 2. What specific characteristics of the abdominal pain should prompt immediate medical evaluation, considering it might very well be indicative of aortic dissection rather than a common gastrointestinal issue?
- 3. A Sudden Stomach Ache, a Life-Threatening Risk: A Case of Aortic Dissection
- 4. Understanding Aortic Dissection & Abdominal Pain
- 5. the Aorta: A Quick Overview
- 6. Why Stomach Ache? The Mimicking Symptoms
- 7. Risk Factors & Causes of Aortic Dissection
- 8. Diagnostic Procedures for Aortic Dissection
- 9. Aortic Dissection Treatment: A Race Against Time
- 10. Real-World Example: A Delayed Diagnosis
A recent case highlights the critical need for clinicians too consider aortic dissection (AD) in the differential diagnosis of patients presenting with ileus-like symptoms, even in the absence of severe pain. this underscores the potential for misdiagnosis and delayed treatment of a life-threatening condition.
The case involved a patient who initially presented with abdominal pain and radiographic findings suggestive of bowel obstruction or ileus. However, a subsequent contrast-enhanced abdominal CT scan revealed a more concerning diagnosis: an intimal flap at the T10-L1 level with an accompanying intramural hematoma extending from the descending aorta into the abdominal aorta. This indicated an uncomplicated Stanford type B aortic dissection.
Further imaging, including CT angiography of the aorta, confirmed the dissection but found no involvement of the aortic arch and no signs of organ damage due to malperfusion. The ileus-like symptoms were attributed to secondary ileus caused by the aortic dissection.
The patient was admitted to the ICU and treated with medications to manage blood pressure and heart rate. Stable during his initial hospital stay, he was discharged on day 7. However, he returned six days later with abdominal pain. Follow-up CT angiography showed no significant changes in the aortic dissection. his condition remained stable with well-controlled blood pressure being managed with medication.
This case serves as a crucial reminder for healthcare professionals.When investigating ileus-like symptoms without a clear cause, aortic dissection should be considered. Early recognition and appropriate diagnostic evaluation are paramount to ensuring timely intervention and improving patient outcomes.
What specific characteristics of the abdominal pain should prompt immediate medical evaluation, considering it might very well be indicative of aortic dissection rather than a common gastrointestinal issue?
A Sudden Stomach Ache, a Life-Threatening Risk: A Case of Aortic Dissection
Understanding Aortic Dissection & Abdominal Pain
Aortic dissection, while relatively rare, is a serious and frequently enough fatal condition frequently misdiagnosed due to its varied presentation. Many patients initially present with symptoms mimicking more common ailments, like a sudden, severe stomach ache. This delay in diagnosis can drastically reduce the chances of survival. This article explores the connection between abdominal pain and aortic dissection, focusing on recognizing the warning signs and the importance of prompt medical attention. We’ll cover aortic dissection symptoms, causes of aortic dissection, and crucial aortic dissection treatment options.
the Aorta: A Quick Overview
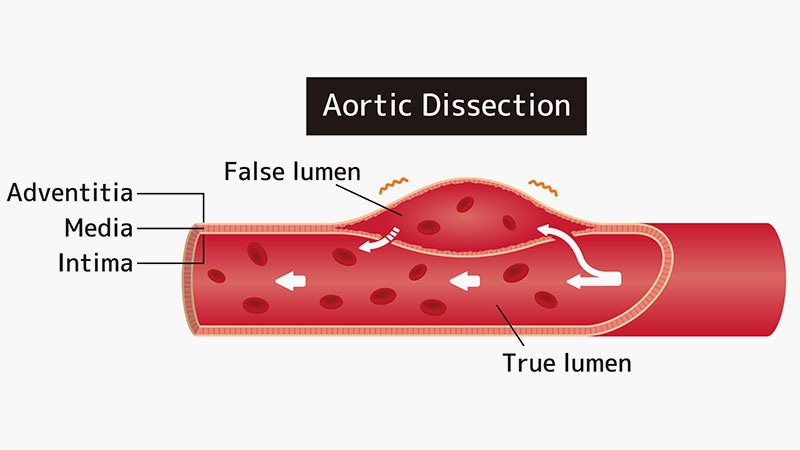
The aorta is the largest artery in the body, originating from the heart and delivering oxygen-rich blood to organs and tissues. It arches down through the chest and into the abdomen.An aortic dissection occurs when a tear develops in the inner layer of the aorta’s wall. Blood then surges through this tear, separating the layers of the aortic wall – a process known as dissection. This can lead to reduced blood flow to vital organs and potentially life-threatening complications.
Why Stomach Ache? The Mimicking Symptoms
The link between aortic dissection and abdominal pain arises because the dissection can occur in the descending thoracic aorta or the abdominal aorta.When this happens, the expanding hematoma (collection of blood) can compress surrounding structures, including abdominal organs.This compression manifests as:
Severe, sudden abdominal pain: Often described as tearing or ripping. This is a key warning sign.
Back pain: Frequently radiating from the chest or abdomen.
Pain that migrates: The location of the pain can shift as the dissection progresses.
Pulse differences: A noticeable difference in pulse strength between arms or legs.
Hypotension (low blood pressure): Resulting from blood loss and reduced organ perfusion.
Neurological symptoms: Such as stroke-like symptoms if blood flow to the brain is compromised.
It’s crucial to differentiate this pain from typical stomach ache causes like indigestion or food poisoning. The sudden onset and severe intensity are red flags.
Risk Factors & Causes of Aortic Dissection
Several factors increase the risk of developing an aortic dissection. Understanding these causes of aortic dissection is vital for preventative measures and early detection:
High Blood Pressure (Hypertension): The most significant risk factor. Chronic hypertension weakens the aortic wall.
Atherosclerosis: Plaque buildup in the arteries, contributing to aortic wall weakening.
Genetic Conditions: Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome affect connective tissue and increase susceptibility.
Bicuspid Aortic Valve: A congenital heart defect.
Family History: Having a family member with aortic dissection increases your risk.
Age: Risk increases with age, notably after 65.
Smoking: Damages blood vessels and contributes to hypertension.
Cocaine Use: Can cause a sudden surge in blood pressure.
Pregnancy: Hormonal changes and increased blood volume can put stress on the aorta.
Diagnostic Procedures for Aortic Dissection
Prompt and accurate diagnosis is paramount. Doctors utilize several imaging techniques to confirm aortic dissection diagnosis:
- CT Scan with Contrast: The gold standard for diagnosing aortic dissection. Provides detailed images of the aorta.
- MRI (Magnetic Resonance Imaging): An choice to CT scans, particularly useful for patients with kidney problems or contrast allergies.
- Transesophageal Echocardiogram (TEE): A probe is inserted into the esophagus to obtain detailed images of the aorta.
- Chest X-ray: May reveal a widened mediastinum (the space in the chest containing the heart and major vessels), suggesting dissection.
Aortic Dissection Treatment: A Race Against Time
Aortic dissection treatment depends on the location and type of dissection (Stanford A or Stanford B).
Stanford Type A Dissection (involving the ascending aorta): Requires immediate surgical intervention. Surgery aims to repair or replace the damaged section of the aorta.
Stanford Type B dissection (involving the descending aorta): Can often be managed medically with medications to control blood pressure and heart rate.However, endovascular repair (using a stent-graft inserted through a catheter) may be necessary in certain cases, especially if there are complications.
Medications used in aortic dissection management include:
Beta-blockers: To lower heart rate and blood pressure.
Calcium channel blockers: Also to control blood pressure.
Vasodilators: To relax blood vessels.
Pain medication: To manage the severe pain.
Real-World Example: A Delayed Diagnosis
I recall a case several years ago where a 58-year-old male presented to the emergency room complaining of severe, sudden *