The Future of Brain Health: Beyond Exercise, Towards Personalized Neuro-Fitness
Imagine a future where your daily routine isn’t just about physical fitness, but about actively ‘tuning’ your brain for optimal performance and resilience. It’s not science fiction. Neurologists are increasingly focused on proactive brain health, and the simple act of exercise – highlighted in the recent 5-Day Brain Health Challenge – is just the beginning. We’re on the cusp of a neuro-fitness revolution, driven by advancements in understanding the brain’s plasticity and the power of personalized interventions.
The Exerkine Effect: Why Movement Matters So Much
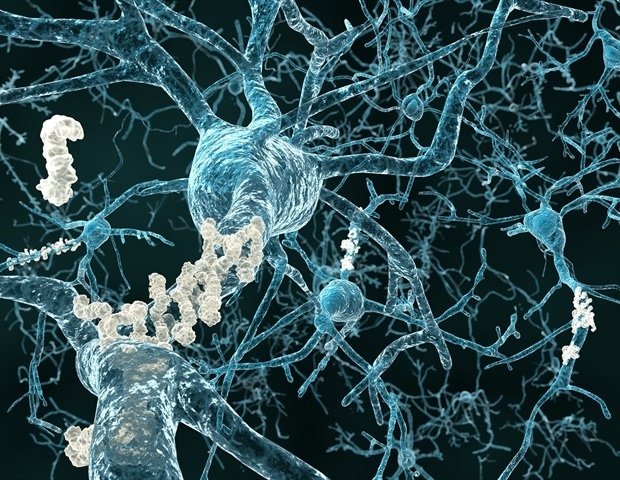
The 5-Day Brain Health Challenge rightly emphasizes exercise as a cornerstone of brain health. Neurologists like Dr. Gregg Day at the Mayo Clinic consistently rank it as “No. 1” for cognitive benefit. But why is exercise so potent? The answer lies in molecules called exerkines. Released during physical activity, these signaling agents travel to the brain, fostering neuron growth, repairing damaged cells, and potentially even stimulating neurogenesis – the birth of new neurons. This isn’t just about feeling good after a workout; it’s about fundamentally reshaping your brain’s architecture.
Beyond exerkines, exercise boosts blood flow, delivering vital oxygen and glucose while clearing out harmful amyloid proteins linked to Alzheimer’s disease. The hippocampus, crucial for learning and memory, is particularly sensitive to these benefits, offsetting the natural age-related shrinkage that begins in our 30s.
The Rise of ‘Cognitive Exercise’ – Beyond the Gym
While any physical activity is beneficial, the future of brain health will likely see a surge in “cognitive exercise” – activities specifically designed to challenge and stimulate the brain *during* physical exertion. Think complex dance routines, obstacle courses requiring strategic thinking, or even augmented reality fitness games that demand problem-solving skills. These combine the benefits of physical activity with targeted cognitive stimulation, potentially amplifying the neuroprotective effects.
Pro Tip: Don’t feel limited to traditional workouts. Gardening, brisk walking while mentally rehearsing a presentation, or even playing a musical instrument while standing can all contribute to your brain’s fitness.
Personalized Neuro-Fitness: The Data-Driven Future
The “best” exercise for your brain isn’t a one-size-fits-all solution. Emerging technologies are paving the way for personalized neuro-fitness plans, tailored to individual needs and genetic predispositions. Wearable sensors, coupled with AI-powered analysis, will soon provide real-time feedback on brain activity during exercise, optimizing routines for maximum cognitive impact.
Imagine a future where your smartwatch doesn’t just track your steps, but also monitors your brainwaves, identifying the types of movement that most effectively enhance focus, memory, or emotional regulation. This data could then be used to create a customized exercise program, maximizing your brain’s potential.
“We’re moving beyond simply *reacting* to cognitive decline,” explains Dr. Anya Sharma, a neuroscientist specializing in personalized medicine. “The goal is to proactively build cognitive reserve – strengthening the brain’s ability to withstand damage and maintain function throughout life.”
The Gut-Brain Connection: A New Frontier
The link between gut health and brain function is gaining increasing attention. Research suggests that the microbiome – the trillions of bacteria living in our gut – plays a crucial role in cognitive health, influencing everything from mood and memory to neuroinflammation.
This opens up exciting possibilities for neuro-fitness. Future interventions may involve personalized dietary plans designed to optimize the gut microbiome, alongside exercise and cognitive training. Prebiotic and probiotic supplements, tailored to an individual’s gut profile, could become a standard part of a brain health regimen.
Expert Insight: “The gut-brain axis is a bidirectional highway,” says Dr. David Perlmutter, author of *Brain Maker*. “What you eat directly impacts your brain, and conversely, your brain influences your gut. Nurturing a healthy gut microbiome is essential for optimal cognitive function.”
Addressing the Equity Gap in Brain Health
While the future of neuro-fitness is promising, it’s crucial to address potential equity gaps. Access to personalized technologies, specialized exercise programs, and even healthy food options may be limited for certain populations.
Efforts must be made to ensure that the benefits of neuro-fitness are accessible to everyone, regardless of socioeconomic status. This could involve developing affordable wearable sensors, creating community-based exercise programs, and promoting nutrition education in underserved areas.
The Role of Gamification and Virtual Reality
Virtual reality (VR) and gamification offer a powerful solution for making neuro-fitness more engaging and accessible. VR environments can simulate challenging cognitive tasks, providing a safe and immersive space for brain training. Gamified exercise programs can motivate individuals to stay active and track their progress, fostering a sense of accomplishment.
Did you know? Studies have shown that VR-based cognitive training can improve memory and attention in older adults, even those with mild cognitive impairment.
Frequently Asked Questions
Q: How much exercise is enough for brain health?
A: Even a few thousand steps a day can reduce dementia risk. Aim for at least 20-30 minutes of moderate-intensity exercise most days of the week, focusing on activities you enjoy.
Q: Can I improve my brain health if I’m already experiencing cognitive decline?
A: Yes! While it’s easier to prevent cognitive decline, exercise and cognitive training can still improve brain function and slow the progression of symptoms. Consult with a healthcare professional for personalized recommendations.
Q: What role does diet play in brain health?
A: A healthy diet rich in fruits, vegetables, whole grains, and healthy fats is crucial for brain health. Focus on foods that support gut health and reduce inflammation.
Q: Are there any risks associated with neuro-fitness technologies?
A: As with any technology, there are potential risks. Data privacy and security are important considerations. It’s also essential to use these technologies responsibly and under the guidance of a healthcare professional.
The future of brain health isn’t about passively waiting for cognitive decline; it’s about actively cultivating a resilient and adaptable brain. By embracing the principles of neuro-fitness – combining exercise, personalized interventions, and a holistic approach to well-being – we can unlock our cognitive potential and live longer, healthier, and more fulfilling lives. What steps will you take today to invest in your brain’s future?
Explore more insights on cognitive enhancement in our comprehensive guide.