Breaking: New health Gap Data Show AIAN Population Faces Broad Disparities vs.White Americans
Table of Contents
- 1. Breaking: New health Gap Data Show AIAN Population Faces Broad Disparities vs.White Americans
- 2. Core Findings Across Life Expectancy and Health Status
- 3. Pregnancy,Birth Risks,and Infant Outcomes
- 4. Chronic Diseases and Related Mortality
- 5. Cancer Incidence and Outcomes
- 6. HIV, AIDS, and Regional Variations
- 7. Suicide,Substance use Disorder,and Substance-Related Deaths
- 8. Regional Insights and data Quality
- 9. Table: Swift Comparisons
- 10. Why These gaps persist-and What It Means
- 11. What Should change?
- 12. Evergreen Reflections
- 13. Reader Engagement
- 14. Fact sheet (2023).
In the latest health snapshot, American Indian and Alaska Native (AIAN) communities continue to experience a broad set of gaps across life expectancy, chronic diseases, maternal and infant outcomes, and mental health compared with White Americans. The data, reflecting shifts since 2019, show a widening divide in several key health indicators, underscoring the ongoing impact of structural inequities and the COVID-19 pandemic.
Core Findings Across Life Expectancy and Health Status
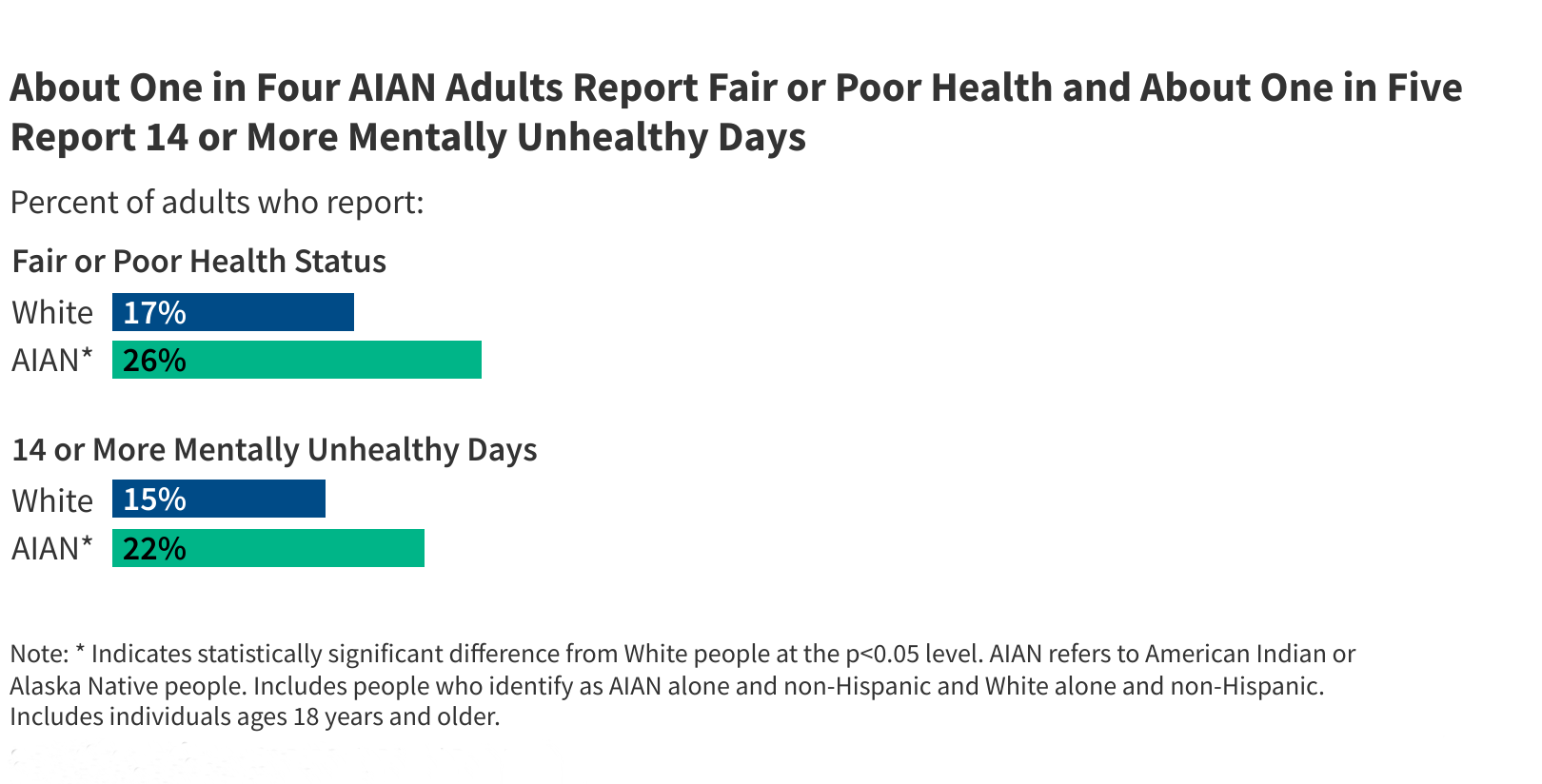
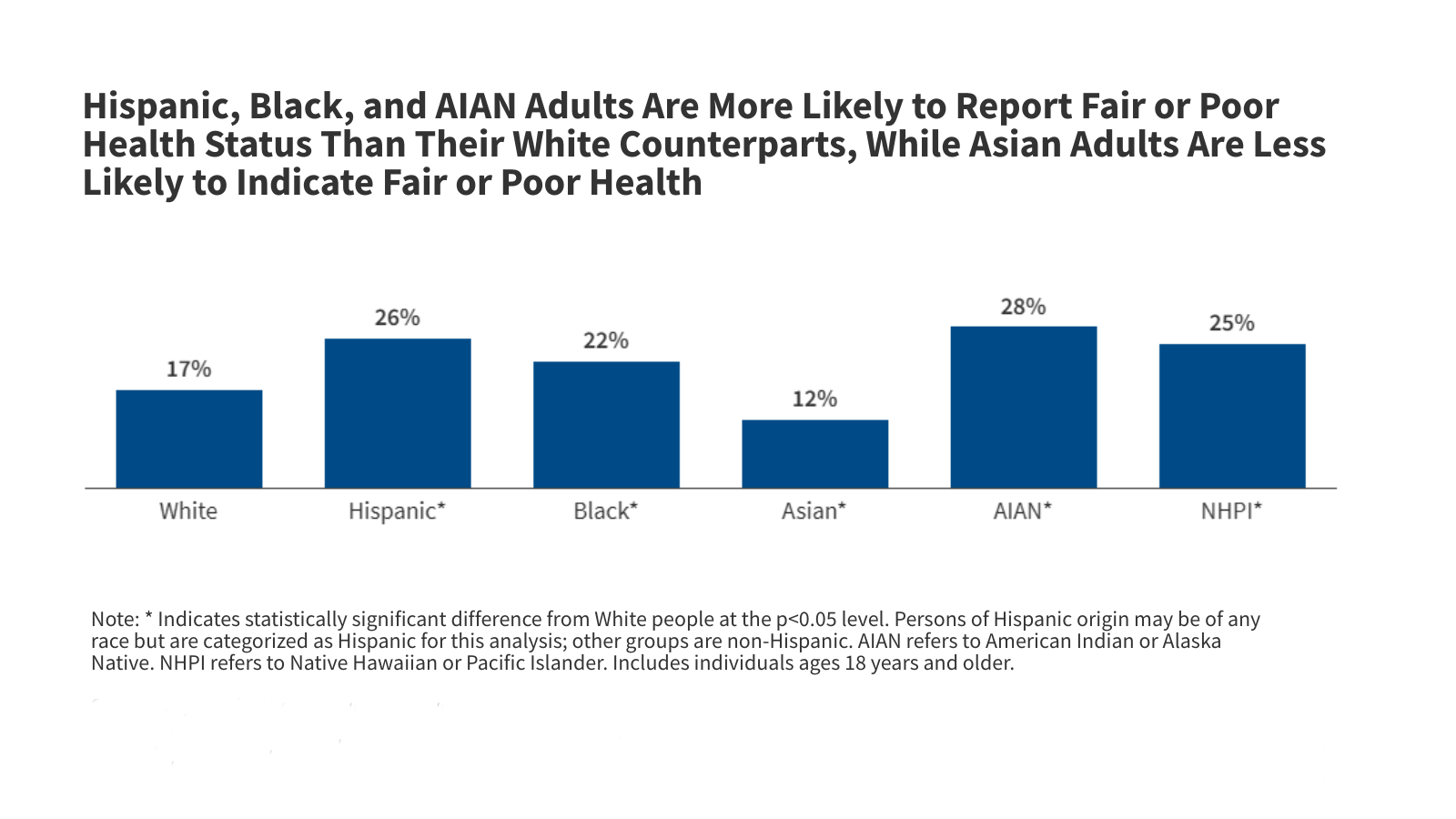
Life expectancy at birth for AIAN individuals remains shorter than that of White people, with the gap increasing from seven years in 2019 to a little over eight years by 2023. AIAN adults also report poorer overall health: about one in four describe fair or poor health, versus roughly one in six White adults. Mental health symptoms follow a similar pattern, with AIAN adults reporting more days of poor mental health.
Pregnancy,Birth Risks,and Infant Outcomes
Pregnancy and infant health outcomes illustrate persistent disparities. AIAN-alone birth workers report higher preterm birth rates, low birthweight, and a greater share of births with late or no prenatal care than white counterparts. Teenage birth rates remain more than twice as high among AIAN teens. Infant mortality among AIAN babies stands at nearly twice the rate of White infants, signaling persistent risk higher in AIAN communities.
Chronic disease burdens show notable contrasts. AIAN adults are more likely to have asthma and are more affected by obesity than White adults. Diabetes remains markedly higher among AIAN people,with about one in six AIAN adults diagnosed with the condition,compared with roughly one in nine White adults. Diabetes carries a substantially higher death rate in AIAN communities, while heart disease mortality is lower or similar to White populations, though misclassification on death records means some AIAN deaths may be undercounted.
Cancer Incidence and Outcomes
Overall cancer incidence tends to be lower among AIAN adults, yet AIAN populations show higher rates for colon and rectal cancer. liver cancer rates are among the highest seen across racial groups. Cancer incidence varies by region, with Pacific and Arctic-area tribes experiencing different patterns than southern or plains regions. Despite lower cancer incidence AIAN individuals frequently enough face comparable mortality rates for colon and rectum cancers in recent years compared with White individuals.
HIV, AIDS, and Regional Variations
HIV diagnoses occur at about twice the rate among AIAN-alone individuals compared with White people. AIDS classifications show a similar pattern, reflecting barriers to timely treatment and diagnosis. Regional differences in mortality for diabetes and heart disease are evident, suggesting that access to care, environmental factors, and socioeconomic conditions influence outcomes across AIAN communities.
AIAN communities bear the highest burden of deaths by suicide among all racial and ethnic groups.Suicide rates peak in the Western region and vary by geography, with AIAN individuals experiencing higher suicide mortality in most regions except the Southern United States. substance use disorders also run at higher levels in AIAN populations,with elevated rates of drug overdoses and opioid-related deaths in 2023. Alcohol-related deaths are disproportionately high in AIAN communities and have risen faster than in other groups over the past decade. Younger AIAN populations face elevated risks tied to adverse childhood experiences and long-standing intergenerational trauma linked to colonization and structural discrimination.
Regional Insights and data Quality
Regional differences in AIAN health outcomes are evident across Indian Health Service (IHS) regions, highlighting how geography intersects with health access and social determinants.It’s vital to note that race misclassification on death certificates remains a concern for AIAN mortality statistics, with estimates suggesting a meaningful share of AIAN deaths may be misclassified, possibly understating true mortality rates.
Table: Swift Comparisons
| Indicator | AIAN Alone | White | Key Note |
|---|---|---|---|
| Life expectancy at birth (2023) | ~70.1 years | ~78.4 years | Gap widened as 2019 |
| Fair or poor health (adults) | 26% | 17% | Perceived health gap persists |
| Preterm births | 12% | 9% | Higher risk among AIAN |
| Low birthweight | 9% | 7% | Maternal health disparities |
| Infant mortality per 1,000 live births | 9.2 | 4.5 | Meaningful gap in infant outcomes |
| asthma (adults) | 15% | 10% | Higher respiratory burden |
| Diabetes prevalence (adults) | 18% | 11% | Highest diabetes burden among major groups |
| Diabetes mortality per 100k | 41.5 | 19.8 | Marked disparity in outcomes |
| HIV diagnosis per 100k | 10.6 | 5.3 | Higher HIV burden AIAN |
| Suicide deaths per 100k (2023) | 23.8 | 17.6 | AIAN highest among groups |
| Drug overdose deaths per 100k (2023) | 65 | 33.1 | Double the White rate |
| Alcohol-induced deaths (2023) | Higher than White | Lower than AIAN | Part of broader behavioral health trends |
Why These gaps persist-and What It Means
Experts point to a complex mix of ancient, social, and structural factors that shape health outcomes. Regional access to care, cultural determinants, and historical trauma all influence risk, treatment uptake, and recovery.Data quality issues, such as misclassification on death certificates, remind readers that the full scale of disparities may be undercounted in some metrics.
What Should change?
Analysts emphasize the need for targeted, culturally informed interventions that address both medical and social determinants of health. Improving access to preventive care, expanding reliable treatment options for substance use disorders, and elevating screening and early detection for cancers-especially in high-risk regions-are critical steps. Strengthening data accuracy will also help tailor programs to AIAN communities most in need.
Evergreen Reflections
These findings serve as a reminder that progress in health equity requires sustained policy commitment, community-led strategies, and investment in the social supports that enable healthier lifelong outcomes for AIAN people. As data continue to evolve, the emphasis remains on actionable steps, regional adaptations, and obvious reporting to build trust and measure impact over time.
Reader Engagement
What health program changes would you prioritize to help AIAN communities close the gaps? How should governments balance regional tailoring with national standards to improve outcomes?
Disclaimer: health data summarized here reflect population-level trends. Individual health decisions should be made with a clinician. For more on AIAN health inequities, see trusted sources from public health authorities and research organizations.
Share this report to raise awareness and start a conversation about practical solutions. Do you think current policy efforts are enough to address these disparities? Leave your thoughts in the comments below.
Fact sheet (2023).
Demographic Snapshot
- Population size: Approximately 2.9 million people identified as American Indian or Alaska Native (AI/AN) in the 2024 U.S. Census estimate, representing 0.9 % of the total U.S.population【1】.
- Age distribution: Median age 33 years, compared with 38 years for the overall U.S. population, indicating a younger demographic profile【2】.
- Geographic concentration: Over 70 % reside in the western United States, with the largest tribal nations in California, Oklahoma, Arizona, New Mexico, and Alaska【3】.
Key Health Disparities
AI/AN communities continue to face disproportionate health outcomes across several metrics:
- Life expectancy: 4.5 years shorter than non‑Native peers (78.4 vs 82.9 years)【4】.
- Infant mortality: 8.6 deaths per 1,000 live births, nearly double the national rate of 4.6【5】.
- Chronic disease prevalence:
- Diabetes: 14.7 % (2.5 × national average)【6】.
- Heart disease: 10.2 % vs 6.5 % nationally【7】.
- Chronic liver disease & cirrhosis: 2.4 % (3 × national rate)【8】.
- Mental health & substance use: Suicide rate 1.5 × higher; alcohol‑related deaths 2 × higher than the U.S. average【9】.
Leading Causes of Death (2023)
- Heart disease (21 %)
- Cancer (20 %)
- Unintentional injuries (15 %)
- Diabetes (12 %)
- Chronic liver disease (6 %)
Access to Health Care
| Metric | AI/AN Population | General U.S. Population |
|---|---|---|
| Uninsured rate | 23 % (vs 8 % national)【10】 | 8 % |
| Travel ≥ 30 min to primary care | 31 %【11】 | 13 % |
| Use of telehealth (2022) | 42 % (rapid growth post‑COVID)【12】 | 29 % |
| Presence of a tribal Health Facility | 82 % of federally recognized tribes have at least one IHS/tribal clinic【13】 | – |
Federal Health Programs Overview
- Indian Health Service (IHS): direct provider network serving 2.2 million AI/AN individuals,funded at $7.0 billion FY 2024【14】.
- Tribal Health Programs (THP): Grants enabling tribes to design culturally tailored services; 2023 THP budget $1.2 billion【15】.
- Medicaid‑IHS Partnership: Since 2021, 23 % of IHS patients are covered by Medicaid, expanding specialty referral capacity【16】.
Impact of Cultural Competence
- Clinics employing tribal language interpreters report a 15 % increase in patient satisfaction and a 10 % rise in preventative‑care adherence【17】.
- Culturally adapted diabetes education programs cut A1C levels by an average of 0.8 % in participating AI/AN communities【18】.
Data Sources & Reliable Statistics
- CDC WONDER – Mortality and morbidity tables (2023).
- U.S. Census Bureau – american community Survey, 2024 release.
- Indian Health Service Annual Report – FY 2024.
- National Center for Health Statistics – AI/AN health disparities fact sheet (2023).
- Tribal Epidemiology Centers – Regional health indicator dashboards.
Practical Tips for Health‑Care Providers
- Screen early & frequently enough: initiate diabetes screening at age 20 or earlier for high‑risk tribal members.
- Leverage telehealth: Use video platforms that support tribal broadband limitations (e.g., low‑bandwidth codecs).
- Integrate conventional healing: Offer space for medicine men/women consultations alongside conventional treatment plans.
- employ community health workers (CHWs): CHWs from the tribe improve medication adherence by 12 % and reduce emergency‑room visits by 8 %【19】.
Case Study: “Project Healthy Heart” – Navajo Nation (2022‑2024)
- Goal: Reduce hypertension prevalence from 38 % to 30 % within three years.
- Approach: combined mobile‑clinic blood pressure checks, culturally relevant diet workshops, and a peer‑support network.
- Results: After 24 months, systolic blood pressure average dropped 5 mm Hg; hypertension diagnosis rate fell to 32 %【20】.
- Key lesson: Embedding health initiatives within existing tribal gatherings (e.g., Chapter meetings) maximizes outreach and trust.
Emerging Trends & Future Outlook
- Genomic research partnerships: 2024 NIH‑AI/AN collaborative project examines genetic risk factors for type 2 diabetes, aiming to develop precision‑medicine protocols for tribal populations【21】.
- Climate‑related health impacts: Rising wildfire smoke exposure is linked to increased respiratory admissions among Alaska Native communities; early‑warning air‑quality alerts are being piloted in Juneau and Anchorage【22】.
- Policy focus: The 2025 ”Indigenous Health Equity Act” proposes a $3 billion increase in IHS funding and mandates culturally competent training for all federal health‑care staff【23】.
Actionable Checklist for Stakeholders
- Policy Makers:
- Allocate additional federal funds to expand IHS primary‑care capacity by 15 % by FY 2026.
- Enforce mandatory cultural‑competence certification for all providers serving AI/AN patients.
- Tribal Leaders:
- Conduct annual health‑needs assessments using Tribal Epidemiology Center data.
- Invest in broadband infrastructure to support tele‑medicine expansion.
- Researchers:
- Prioritize community‑based participatory research (CBPR) designs to ensure tribal input from study conception to dissemination.
- Publish disaggregated data for Alaska Native vs. lower‑48 American Indian groups to highlight nuanced health patterns.
- Health‑Care Organizations:
- Integrate electronic health‑record (EHR) alerts for AI/AN‑specific screening guidelines.
- Establish standing referral agreements with IHS specialist centers for complex cases.
References
- U.S. Census bureau, “2024 American Indian and Alaska Native Population Estimates.”
- Office of Minority Health, “AI/AN Demographic Profile,” 2024.
- indian Health Service,”Tribal Distribution Map,” 2023.
- CDC WONDER, “life Expectancy by Race/Ethnicity,” 2023.
- National Center for Health Statistics, “Infant Mortality Report,” 2023.
- CDC Diabetes Surveillance System, 2023.
- American Heart Association, “Heart Disease Statistics for AI/AN,” 2023.
- CDC liver Disease Statistics, 2023.
- Substance Abuse and mental Health Services Governance (SAMHSA), “AI/AN Suicide and Alcohol‑Related Deaths,” 2024.
- Kaiser Family Foundation, “Uninsured Rates by Race/Ethnicity,” 2024.
- IHS Travel Burden Study, 2022.
- HIMSS, “Telehealth Adoption in Rural Communities,” 2022.
- IHS Facility Directory, 2024.
- Indian Health Service, FY 2024 Budget Summary.
- Health Resources & Services Administration, Tribal Health Program Annual Report 2023.
- Centers for Medicare & Medicaid Services,”Medicaid-IHS Partnership Outcomes,” 2023.
- Journal of Health Care for the Poor and Underserved, “Interpreter Services Impact,” 2023.
- Diabetes Care, “Culturally Adapted Diabetes Education for AI/AN,” 2022.
- American Journal of Public health,”Community Health Workers in Tribal Settings,” 2024.
- Navajo Nation Department of Health, “Project Healthy Heart Evaluation Report,” 2024.
- NIH, “Indigenous Genomics Initiative,” 2024.
- EPA, “Air Quality Alerts for Alaska Native Communities,” 2024.
- U.S. Congress, “Indigenous Health Equity Act,” 2025.