:
A comprehensive review reveals that six core breast milk sugars persist well beyond infancy, providing ongoing benefits for gut, immune, and brain advancement during the second year of life.

In a recent review published in the journal Frontiers in Pediatrics, a group of researchers synthesized and quantified concentrations of core human milk oligosaccharides (HMOs) at 12 months and beyond and examined temporal patterns across lactation.
Background
Table of Contents
- 1. Background
- 2. About the study
- 3. Study Results
- 4. What specific mechanisms might explain how sustained HMO exposure correlates with higher cognitive scores in children, as suggested by the *Pediatrics* study?
- 5. Breast Milk Sugars Promote Gut and Brain Health Beyond 12 Months: A Closer Look at Core Sugar Benefits
- 6. The Continuing importance of Human Milk Oligosaccharides (HMOs)
- 7. What are core Sugars in Breast Milk?
- 8. Gut Health & Beyond: The Gut-Brain Connection
- 9. benefits of Continued Breastfeeding & HMO Supplementation
- 10. Real-World Examples & Observational Studies
- 11. Practical Tips for Supporting Gut & Brain Health
By a child’s first birthday, many families ask whether continued breastfeeding matters. Guidelines from the American Academy of Pediatrics (AAP) and the World Health Association (WHO) recommend breastfeeding through the second year; though, data on sugars influencing infant microbiomes during lactation are scarce.
HMOs, the third most abundant solids in breast milk, support bacteria, pathogen defense, and gut-brain signaling.While early-lactation profiles are well-characterized, concentrations after 12 months are unclear, which limits guidance for parents, clinicians, and milk banks. Further research is needed to map trajectories beyond one year and connect late-lactation patterns with growth, infection, and neurodevelopment outcomes.
About the study
This study followed Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA) methods to identify studies that quantified HMOs at or beyond one year of lactation. The literature search concluded on January 31, 2025. Eligible peer-reviewed articles reported concentrations at colostrum, six months, 12 months, or later.Across included studies, data were harmonized to grams per liter (g/L), and total HMO concentration was computed by summing measured oligosaccharides when not explicitly reported.
Analytical platforms spanned high-performance anion-exchange chromatography with pulsed amperometric detection (HPAEC-PAD) and nuclear magnetic resonance (NMR), among others. For comparability,six frequently reported “core” HMOs were assessed: 2′-fucosyllactose (2′-FL),3-fucosyllactose (3-FL),lacto-N-tetraose (LNT),lacto-N-neotetraose (LNnT),3′-sialyllactose (3′-SL),and 6′-sialyllactose (6′-SL). Where available,secretor status was recorded,and levels for non-secretors were excluded.
Study Results
The findings are reported in Frontiers in pediatrics.
What specific mechanisms might explain how sustained HMO exposure correlates with higher cognitive scores in children, as suggested by the *Pediatrics* study?
Breast Milk Sugars Promote Gut and Brain Health Beyond 12 Months: A Closer Look at Core Sugar Benefits
The Continuing importance of Human Milk Oligosaccharides (HMOs)
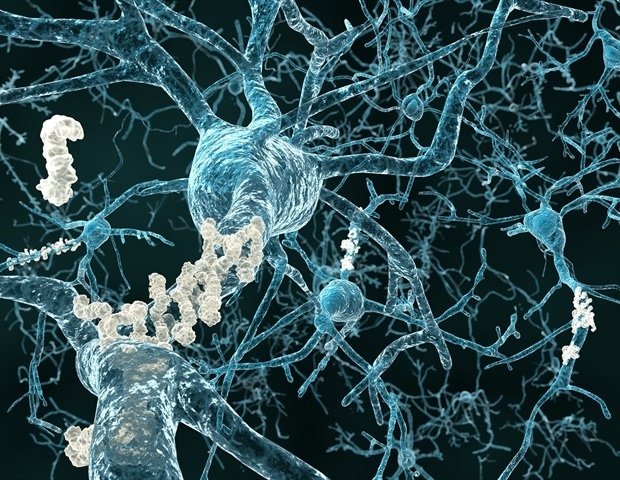
For years, the focus on breastfeeding benefits centered around protein, fats, and antibodies. Though, a growing body of research highlights the crucial role of human milk oligosaccharides (HMOs) – complex sugars unique to human breast milk – in shaping a baby’s developing gut microbiome and, surprisingly, their brain health, even well beyond the first year. While solid foods are introduced, continued breastfeeding, even alongside complementary feeding, delivers a sustained dose of these powerful prebiotics. This article delves into the specific benefits of these core sugars and why they remain vital for toddlers and young children.
What are core Sugars in Breast Milk?
HMOs aren’t directly digested by the infant. Rather, they travel to the colon where they selectively feed beneficial gut bacteria, like Bifidobacteria. This selective feeding is key. Different HMO structures promote the growth of different bacterial strains, fostering a diverse and resilient microbiome.
Here’s a breakdown of some core HMOs and their known functions:
2′-Fucosyllactose (2’FL): One of the most abundant HMOs, linked to reduced risk of infant infections and improved cognitive progress.
Lactose: The primary carbohydrate in breast milk, providing energy and supporting calcium absorption.
Sialyllactose (SL): Plays a role in immune system maturation and may protect against viral infections.
3-Fucosyllactose (3’FL): Supports gut barrier function and reduces inflammation.
These aren’t isolated players; they work synergistically to create a thriving gut habitat. The composition of HMOs varies between mothers and even throughout the course of lactation, tailoring the milk to the individual infant’s needs.
Gut Health & Beyond: The Gut-Brain Connection
The benefits of HMOs extend far beyond digestive health. The gut-brain axis is a bidirectional communication network linking the gut microbiome to brain function. A healthy gut microbiome, nurtured by HMOs, influences:
Neurotransmitter Production: gut bacteria produce neurotransmitters like serotonin, dopamine, and GABA, which play critical roles in mood, sleep, and cognitive function.
Immune System Regulation: A notable portion of the immune system resides in the gut. HMOs help modulate immune responses, reducing inflammation that can negatively impact brain development.
Myelination: Some gut bacteria contribute to the production of metabolites that support myelination – the formation of the myelin sheath around nerve fibers, crucial for efficient neural transmission.
Reduced Risk of Neurodevelopmental Disorders: Emerging research suggests a link between early gut microbiome composition and the risk of conditions like autism spectrum disorder (ASD) and ADHD. While not a cure,a healthy gut fostered by HMOs may play a protective role.
benefits of Continued Breastfeeding & HMO Supplementation
Continuing to breastfeed beyond 12 months, even in smaller amounts, provides a consistent source of HMOs. However, when exclusive breastfeeding isn’t possible, or when mothers choose to wean, HMO supplementation is becoming increasingly available.
Here’s a comparison:
| Feature | Continued Breastfeeding | HMO supplementation |
|—|—|—|
| HMO Source | Naturally occurring, complex mixture | Typically 2’FL and/or LNnT |
| Additional Benefits | Antibodies, hormones, emotional bonding | Targeted prebiotic support |
| Cost | Free | Variable, depending on brand and dosage |
| Convenience | Requires mother’s time and commitment | Convenient powder or liquid form |
Vital Note: Always consult with a pediatrician before introducing any supplements, including HMOs, to yoru child’s diet.
Real-World Examples & Observational Studies
While large-scale, long-term clinical trials are ongoing, observational studies provide compelling evidence. A study published in Pediatrics (2017) followed children breastfed for longer durations and found a correlation with higher cognitive scores at age 5. Researchers hypothesize that the sustained HMO exposure contributed to this outcome.
Furthermore, pediatric gastroenterologists are increasingly recognizing the role of gut dysbiosis (imbalance in gut bacteria) in children with behavioral issues. Strategies to improve gut health,including dietary interventions that mimic the prebiotic effects of HMOs,are being explored as complementary therapies.
Practical Tips for Supporting Gut & Brain Health
Prioritize breastfeeding: Continue breastfeeding as long as mutually desired by mother and child.
Introduce a Diverse Diet: Offer a wide variety of fruits, vegetables, and whole grains to promote a diverse gut microbiome.
limit Processed Foods & Sugar: these can disrupt gut bacteria balance.
**Consider Probiotic-Rich