Sorbitol: The ‘Healthy’ Sugar Substitute Linked to Liver Issues, New research Reveals
Table of Contents
- 1. Sorbitol: The ‘Healthy’ Sugar Substitute Linked to Liver Issues, New research Reveals
- 2. Could reducing sorbitol intake be a preventative measure for individuals with risk factors for NAFLD,such as obesity or diabetes?
- 3. The Link Between Sorbitol and Increased Risk of Steatotic Liver Disease
- 4. Understanding Steatotic Liver Disease (NAFLD/NASH)
- 5. How Sorbitol Impacts Liver Health
- 6. Sorbitol Sources & Daily Intake considerations
- 7. Identifying Individuals at Higher Risk
- 8. Diagnostic Tools & Monitoring
- 9. Dietary Strategies & Management
St. Louis, MO – For years, sugar alcohols like sorbitol have been marketed as healthier alternatives to refined sugar, often found in “sugar-free” candies, gums, and naturally occurring in fruits like apples and peaches. However, groundbreaking new research from Washington University in St. Louis challenges this assumption, suggesting sorbitol may not be as harmless as previously believed.
The study, published in Science Signaling, builds upon previous work by Professor Gary Patti and his team detailing the detrimental effects of fructose on the liver and othre bodily systems. Patti’s earlier research demonstrated how fructose can fuel cancer cell growth and contribute to steatotic liver disease, a condition affecting approximately 30% of adults globally.
The latest findings reveal a surprising connection: because sorbitol is chemically “one transformation away from fructose,” it can trigger similar harmful effects. experiments conducted on zebrafish showed that sorbitol, whether consumed directly or produced naturally in the gut from glucose, is ultimately converted into fructose in the liver.
“There are many roads to fructose in the liver, and potential detours,” Patti explained, highlighting the complex interplay between sorbitol and glucose consumption, and the crucial role of gut bacteria.
While sorbitol metabolism has historically been linked to high glucose levels in pathological conditions like diabetes, the research demonstrates that even in healthy individuals, glucose levels in the gut can rise sufficiently after eating to initiate sorbitol production.
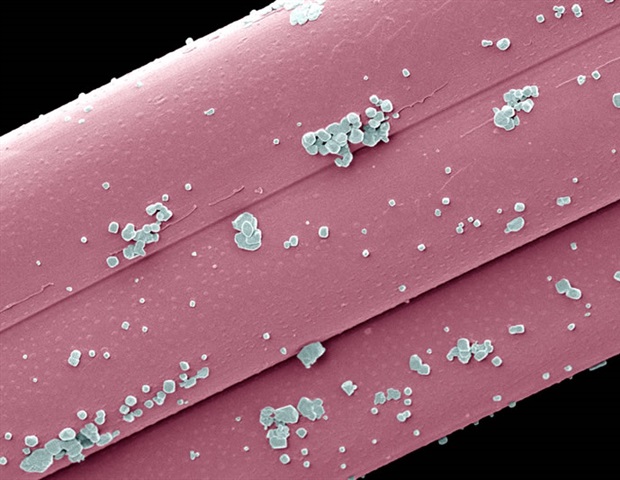
However, the impact of sorbitol isn’t uniform. The presence of specific Aeromonas bacterial strains in the gut can effectively degrade sorbitol into a harmless byproduct. “It can be produced in the body at significant levels. But if you have the right bacteria, turns out, it doesn’t matter,” Patti stated.
The problem arises when individuals lack these beneficial bacteria, allowing sorbitol to bypass degradation and travel to the liver, where it’s converted into a fructose derivative.
The research indicates that gut bacteria generally handle modest levels of sorbitol, such as those found in fruit. Though, excessive glucose intake – leading to increased glucose-derived sorbitol – or high dietary sorbitol consumption can overwhelm the gut’s capacity, triggering the problematic conversion in the liver.
This discovery raises critical questions about the true health benefits of option sweeteners, particularly for individuals with diabetes and other metabolic disorders who rely on “sugar-free” products.Further examination is needed to determine whether these sweeteners truly offer a healthy alternative to traditional table sugar.
Could reducing sorbitol intake be a preventative measure for individuals with risk factors for NAFLD,such as obesity or diabetes?
The Link Between Sorbitol and Increased Risk of Steatotic Liver Disease
Understanding Steatotic Liver Disease (NAFLD/NASH)
Steatotic liver disease,encompassing Non-Alcoholic Fatty Liver Disease (NAFLD) and its more severe form,Non-Alcoholic Steatohepatitis (NASH),is a growing global health concern. Characterized by an accumulation of fat in the liver, it can progress to cirrhosis, liver failure, and even liver cancer. While often linked to obesity, diabetes, and metabolic syndrome, emerging research highlights a potential, often overlooked, contributor: excessive sorbitol consumption. This article explores the connection between sorbitol, fatty liver, and the increasing risk of NAFLD, offering insights into prevention and management.
How Sorbitol Impacts Liver Health
Sorbitol, a sugar alcohol commonly found in fruits like apples, pears, and peaches, and widely used as a sweetener in sugar-free products (gum, candies, medications), isn’t fully absorbed by the small intestine.This incomplete absorption leads to several metabolic consequences that can strain the liver.
* Fructose Metabolism: Sorbitol is metabolized primarily in the liver via the sorbitol pathway, ultimately converting to fructose. Excessive fructose intake is strongly linked to de novo lipogenesis – the creation of new fat in the liver. This process directly contributes to liver fat accumulation.
* Osmotic Effect: Because sorbitol isn’t fully absorbed, it draws water into the intestines, potentially causing bloating, gas, and diarrhea. This osmotic effect can also disrupt gut microbiota balance.
* Gut Microbiome Disruption: An imbalanced gut microbiome (dysbiosis) is increasingly recognized as a key player in NAFLD growth. Sorbitol can feed certain bacteria, leading to an overgrowth of species that promote inflammation and increase intestinal permeability – frequently enough referred to as “leaky gut.”
* Increased Oxidative Stress: The metabolic processes involved in sorbitol breakdown can generate reactive oxygen species (ROS), contributing to oxidative stress in the liver. Oxidative stress damages liver cells and exacerbates inflammation.
Sorbitol Sources & Daily Intake considerations
Many are unaware of the hidden sorbitol in their diet. Beyond naturally occurring sources, it’s prevalent in:
* Sugar-Free Foods: Look for sorbitol on ingredient lists of sugar-free candies, chewing gum, baked goods, and desserts.
* Medications: Sorbitol is used as an excipient (inactive ingredient) in liquid medications, syrups, and some tablets.
* Diet Sodas & “Healthy” Drinks: Some beverages marketed as low-sugar or healthy utilize sorbitol as a sweetener.
* Fruit Juices & Concentrates: While fruits contain sorbitol naturally, concentrated forms like juice can deliver a notable dose.
Recommended Daily Intake: While there isn’t a universally agreed-upon limit, consuming over 50 grams of sorbitol daily can cause gastrointestinal distress. For individuals predisposed to liver disease, even lower amounts might potentially be problematic.
Identifying Individuals at Higher Risk
Certain populations are more vulnerable to the negative effects of sorbitol on liver health:
* Individuals with Pre-existing NAFLD: Sorbitol can accelerate disease progression.
* People with Fructose Malabsorption: Those who struggle to metabolize fructose will experience amplified effects from sorbitol’s conversion.
* Individuals with Insulin Resistance: Insulin resistance impairs the liver’s ability to regulate fat metabolism, making it more susceptible to sorbitol-induced fat accumulation.
* Those with Gut Dysbiosis: An already imbalanced gut microbiome is more easily disrupted by sorbitol.
* Individuals on High-Fructose Diets: Combining sorbitol with other fructose sources (high-fructose corn syrup) creates a synergistic effect, increasing liver stress.
Diagnostic Tools & Monitoring
Detecting early signs of steatosis is crucial. Common diagnostic tools include:
- Liver Function Tests (LFTs): Blood tests that assess liver enzyme levels (ALT, AST). Elevated levels can indicate liver damage.
- Ultrasound: A non-invasive imaging technique to visualize the liver and detect fat accumulation.
- fibroscan: A specialized ultrasound that measures liver stiffness, indicating the degree of fibrosis (scarring).
- Liver Biopsy: The gold standard for diagnosing NASH, involving a tissue sample analysis.
Regular monitoring of LFTs and imaging studies is recommended for individuals with risk factors or suspected sorbitol-related liver issues.
Dietary Strategies & Management
Managing sorbitol intake is a key component of a liver-healthy lifestyle:
* Read Food Labels Carefully: Become a label detective and avoid products with sorbitol, particularly if you have risk factors.
* Limit Sugar-Free Products: Reduce consumption of sugar-free candies, gum, and baked goods.
* Choose Whole Fruits Over Juices: Whole fruits provide fiber and nutrients,mitigating some of sorbitol’s negative effects.
* Reduce Fructose Intake: Limit high-fructose corn syrup and other fructose-rich foods.
* Support Gut Health: Consume probiotic-rich foods (yogurt, kefir