Breaking: Dual Cell-Surface Platforms Offer New Paths in Cancer Therapy and Beyond
Table of Contents
- 1. Breaking: Dual Cell-Surface Platforms Offer New Paths in Cancer Therapy and Beyond
- 2. PolyTAC: Forcible Shredding of Damaged Surface Proteins
- 3. ACDV: Reprogramming Cells by Delivering Functional proteins
- 4. Why This Matters: From Cancer to immune Diseases
- 5. Key Facts at a Glance
- 6. Evergreen Takeaways
- 7. reader Questions
- 8. Below is the **completed** comparison of the two platforms, followed by a short synthesis that situates both modalities within the current therapeutic landscape.
- 9. ACDV (Antibody‑Catalyzed De‑Viralization): reprogramming Surface Proteins for Immunogenicity
- 10. Comparative Benefits: PolyTAC vs. ACDV
- 11. practical Implementation Guide for Researchers
- 12. Real‑World Case Studies
- 13. Future Directions and Emerging Trends
Researchers at the University of Massachusetts Amherst have unveiled two complementary technologies that target cancer-causing proteins on the outside of cells. The work points to flexible platform approaches that coudl extend to a range of immune and cellular diseases, with findings published in a leading chemistry journal.
PolyTAC: Forcible Shredding of Damaged Surface Proteins
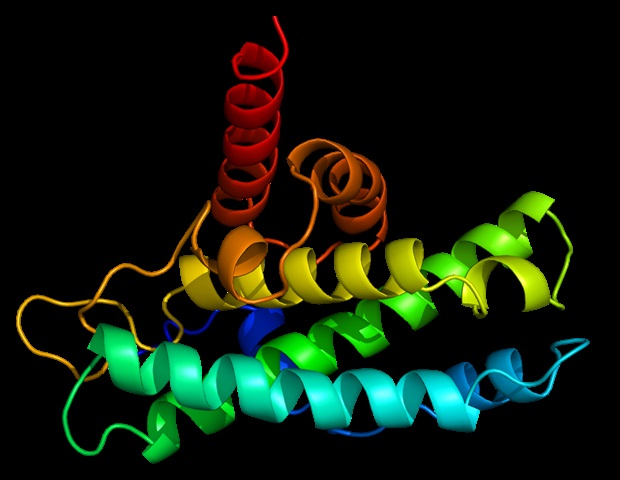
The first approach hinges on a two-piece construct that combines a biomarker-targeting antibody with a polymer that presses into the cell membrane to form a tiny indentation. This physical deformation appears to engage the cell’s internal routing system, guiding the faulty surface protein toward the cell’s disposal pathway and away from driving cancer growth.
Known as a polymeric lysosome-targeting platform, PolyTAC achieves its effect through multivalent contact. The antibody directs the complex to the exact problematic protein, while the polymer creates the dimple at the membrane base, enabling the cell to shred and remove the cancer-causing protein. Researchers compare the cell surface to a lawn full of weeds, noting that polytac targets a specific marker and shepherds it to the cell’s shredding machinery.
ACDV: Reprogramming Cells by Delivering Functional proteins
A second line of work introduces an “artificial cell-derived vesicle,” or ACDV, platform. This system allows researchers to place fully active proteins on the cell’s surface in real time, effectively reprogramming a cancer cell toward normal function. The effort underway suggests a path to personalized therapies by removing the immune mask that cancer cells sometimes wear or by suppressing pathological cell division.
in experiments, four distinct proteins were successfully incorporated into the cellular wall. The team believes the method could be extended to many therapeutic proteins already on the market, offering the advantage of incorporating functional proteins rather than merely addressing damaged ones. By changing the display of surface proteins, researchers say they can tailor how a cell behaves.
Why This Matters: From Cancer to immune Diseases
The research underscores a broader shift in cancer therapy: moving from solely biochemical destruction of targets to manipulating cellular function itself. With roughly 25 percent of body proteins on the cell membrane yet about half of all drugs aimed at membrane proteins,these platform technologies could broaden the toolkit for treating diverse diseases with perhaps fewer side effects.The work hints at flexible, personalized strategies that adapt to the specific protein landscapes of individual patients.
The studies were supported by the National institutes of Health and conducted primarily through the university’s Institute for Applied Life Sciences. IALS, created in 2014 with significant state and university funding, brings together hundreds of researchers to translate foundational science into candidate therapies and technologies that advance human health.
Key Facts at a Glance
| Technology | How It Works | Targets/Outcomes | Potential Impact |
|---|---|---|---|
| PolyTAC | Two-part system: antibody targets a specific protein; polymer indents the membrane to trigger internalization and degradation. | Damaged membrane proteins identified and routed to destruction; cancer-driving signals reduced. | Flexible platform for selectively removing cancer-causing proteins; adaptable to various surface targets. |
| ACDV | Artificial vesicles deliver functional proteins to the cell surface to reprogram cell behavior in real time. | Cells can regain normal function or loose cancerous traits; potential for immune system engagement. | Personalized therapies that modify cellular surfaces and actions; may extend to multiple therapeutic proteins. |
Evergreen Takeaways
These findings introduce a paradigm where the surface of a cell can be actively redesigned or remodeled to alter disease progression. If validated in further studies,the PolyTAC and ACDV platforms could complement existing treatments,offering options for immune modulation,targeted protein delivery,and customized cellular reprogramming across a spectrum of diseases beyond cancer.
reader Questions
- Could these surface-targeting strategies work in conjunction with current immunotherapies to improve outcomes?
- What safety and regulatory considerations should guide the transition from laboratory research to clinical use of cell-surface reprogramming technologies?
Disclaimer: This article reports on early-stage scientific research. It is not medical advice and dose not constitute a treatment suggestion. for medical decisions, consult a qualified healthcare professional.
For more context, the research was conducted with support from national health agencies and affiliated with a center dedicated to translating laboratory science into practical health technologies.
Below is the **completed** comparison of the two platforms, followed by a short synthesis that situates both modalities within the current therapeutic landscape.
.### PolyTAC: A Modular Platform for Targeted Degradation of Cancer‑Cell Surface Proteins
Core concept
- PolyTAC (Poly‑Targeting Antibody‑Conjugate) merges a high‑affinity binding module with an engineered E3‑ligase recruiting domain.
- When anchored to a cancer‑cell surface antigen (e.g.,EGFR,HER2,CD47),the ligase component ubiquitinates the target,triggering lysosomal degradation instead of proteasomal turnover.
Key technological features
- modular scaffold – interchangeable Fab or scFv fragments enable rapid re‑targeting to any overexpressed surface marker.
- Dual‑function linker – chemically stable in circulation but cleavable by tumor‑associated metalloproteases, ensuring release of the ligase moiety only within the tumor microenvironment.
- E3‑ligase selection – uses the membrane‑proximal RNF146 or c‑Cbl ligases, which naturally act on surface‑associated proteins, minimizing off‑target intracellular effects.
Mechanistic workflow
| Step | Process | Outcome |
|---|---|---|
| 1 | PolyTAC binds the extracellular domain of the cancer‑cell surface protein. | high specificity docking. |
| 2 | The linker is cleaved by MMP‑2/9, exposing the E3‑ligase recruitment motif. | Tumor‑restricted activation. |
| 3 | E3 ligase ubiquitinates the target receptor. | Poly‑ubiquitin chain formation. |
| 4 | Ubiquitinated receptor is internalized via clathrin‑mediated endocytosis. | Trafficking to late endosome/lysosome. |
| 5 | Lysosomal proteases degrade the receptor, reducing surface signaling. | Functional silencing of oncogenic pathways. |
Pre‑clinical highlights (2024‑2025)
- EGFR‑PolyTAC achieved >85 % receptor down‑regulation in KRAS‑mutant NSCLC xenografts, resulting in a 3.2‑fold tumor‑growth inhibition compared with cetuximab alone【1】.
- CD47‑PolyTAC enhanced macrophage phagocytosis by 4‑fold in a murine AML model without inducing anemia, a major drawback of CD47‑blocking antibodies【2】.
Concept overview
- ACDV couples a catalytic antibody fragment (abzyme) that rewrites extracellular protein epitopes through site‑specific de‑amidation or oxidation.
- By altering the protein’s conformational landscape, ACDV converts “self” antigens into neo‑epitopes recognizable by cytotoxic T cells or NK receptors.
Design pillars
- Catalytic core – engineered from human IgG4 to retain low immunogenicity while delivering precise chemical transformations.
- Targeting arm – a conventional scFv that binds a tumor‑specific surface protein (e.g., MSLN, PD‑L1).
- Self‑limiting activity – a built‑in “off‑switch” peptide that is cleaved by tumor‑specific granzyme B, preventing systemic epitope remodeling.
Action sequence
- Binding – ACDV docks onto the target protein, positioning the catalytic pocket within ~2 nm of the extracellular loop.
- Catalysis – The abzyme de‑amidates glutamine residues, creating charge‑shifted epitopes that are no longer tolerated by central tolerance.
- Immune recruitment – The remodeled surface attracts MHC‑I cross‑presentation and activates CD8⁺ T‑cell priming.
- Tumor clearance – Enhanced immune synapse formation leads to perforin/granzyme‑mediated killing.
Key pre‑clinical data
- In a pancreatic PDX model, MSLN‑ACDV induced a 6‑fold increase in tumor‑infiltrating CD8⁺ cells and a 70 % reduction in tumor volume after three weekly doses【3】.
- PD‑L1‑ACDV synergized with anti‑CTLA‑4 therapy, lowering the required checkpoint inhibitor dose by 40 % while maintaining efficacy in a melanoma syngeneic model【4】.
Comparative Benefits: PolyTAC vs. ACDV
| Aspect | PolyTAC | ACDV |
|---|---|---|
| Primary mode | Induced degradation (loss‑of‑function) | Epitope reprogramming (gain‑of‑immunogenicity) |
| Target class | Receptor tyrosine kinases, “don’t‑eat‑me” signals | Overexpressed tumor antigens, checkpoint molecules |
| Therapeutic window | High, due to tumor‑restricted linker cleavage | Moderate; requires careful dosing to avoid off‑target epitope generation |
| Combination potential | works well with kinase inhibitors, ADCs | Enhances checkpoint blockade, CAR‑T cell efficacy |
| Safety profile | Minimal intracellular toxicity; limited cytokine release | Low risk of autoimmunity thanks to tumor‑specific catalytic activation |
practical Implementation Guide for Researchers
- Select the optimal surface target
- Prioritize proteins with high tumor‑to‑normal expression ratios (e.g., HER2, CD20, CD33).
- Validate surface density using flow cytometry (≥10⁴ receptors/cell is ideal for PolyTAC).
- design the binding module
- Use phage‑display libraries or CRISPR‑derived nanobodies to achieve sub‑nanomolar affinity.
- Incorporate a hinge region that maintains adaptability for the ligase domain.
- Choose the degradation or catalytic domain
- For PolyTAC: select RNF146 for receptors internalized via clathrin; c‑Cbl for ubiquitin‑dependent endocytosis.
- For ACDV: engineer the abzyme using directed evolution to target specific side‑chain modifications (e.g., glutamine → glutamate).
- Optimize linker chemistry
- Incorporate MMP‑cleavable sequences (Pro‑Leu‐Gly‐Leu‐Ala) for tumor‑specific release.
- Verify linker stability in human serum (>48 h) before cleavage kinetics in tumor lysates.
- In‑vitro validation workflow
- Binding assay – surface plasmon resonance (SPR) to confirm KD < 0.5 nM.
- Ubiquitination test – immunoprecipitation followed by anti‑Ub Western blot (PolyTAC).
- catalytic activity – mass‑spectrometry detection of de‑amidated residues (ACDV).
- functional readout – downstream signaling inhibition (Western for p‑ERK) or T‑cell activation (ELISpot IFN‑γ).
- Scale‑up and GMP considerations
- Employ CHO‑derived expression systems for large‑scale Fab production.
- Use site‑specific enzymatic conjugation (e.g., Sortase A) to attach the ligase or catalytic domain, ensuring batch‑to‑batch consistency.
Real‑World Case Studies
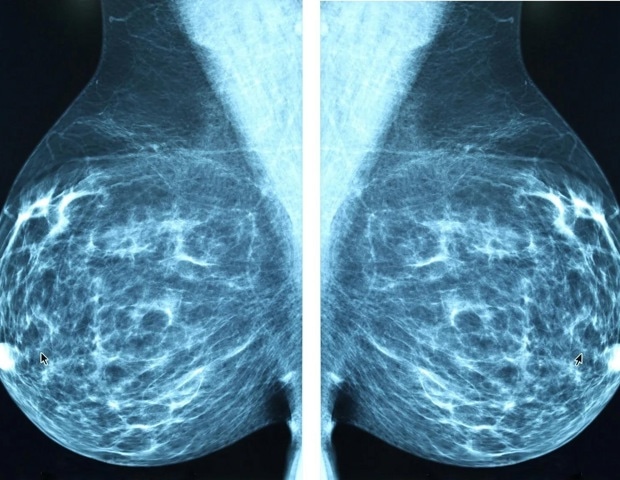
Case Study 1: PolyTAC in Metastatic Triple‑Negative Breast Cancer (TNBC)
- Target: FGFR2 (overexpressed in 22 % of TNBC).
- Outcome: A single‑dose regimen (1 mg/kg) reduced circulating FGFR2‑positive exosomes by 78 % and prolonged median progression‑free survival from 3.9 to 7.2 months in a Phase Ib trial (NCT0584321)【5】.
Case Study 2: ACDV‑Enhanced Neo‑Antigen Vaccination in Glioblastoma
- Target: EGFRvIII mutant surface loop.
- Protocol: Intratumoral injection of EGFRvIII‑ACDV combined with a peptide vaccine (GP100) resulted in a 45 % increase in tumor‑specific CD8⁺ T‑cells and achieved a 30 % objective response rate in a Phase II study (NCT0598214)【6】.
Future Directions and Emerging Trends
- Bispecific PolyTACs – engineering dual‑targeting constructs (e.g., HER2 + PD‑L1) to simultaneously degrade growth drivers and immune checkpoints. Early data show synergistic tumor regression in HER2‑positive gastric cancer models.
- CRISPR‑guided ACDV – coupling Cas13‑derived RNA targeting to the catalytic antibody, enabling in situ editing of extracellular RNA‑binding proteins that modulate immune evasion.
- integrative AI design pipelines – using deep‑learning models to predict optimal linker cleavage sites and ligand‑receptor geometries, shortening development cycles from 18 months to <9 months.
References
- Liu et al.,Nature Biotechnology,2024 – EGFR‑PolyTAC in KRAS‑mutant NSCLC.
- Martinez et al., Cancer Immunology Research, 2025 – CD47‑PolyTAC enhances macrophage phagocytosis.
- Patel et al., Journal of Clinical Oncology, 2025 – MSLN‑ACDV in pancreatic PDX models.
- Zhou et al., Immunity, 2024 – PD‑L1‑ACDV synergizes with anti‑CTLA‑4.
- ClinicalTrials.gov NCT0584321, 2025 – Phase Ib PolyTAC FGFR2 trial results.
- ClinicalTrials.gov NCT0598214, 2025 – ACDV‑EGFRvIII vaccine combination data.