Breath Sensor offers Rapid, Non-Invasive Diabetes Diagnosis
Table of Contents
- 1. Breath Sensor offers Rapid, Non-Invasive Diabetes Diagnosis
- 2. The Science Behind the Breath Test
- 3. Laser-Induced Graphene: A Key Component
- 4. Overcoming Technical Hurdles
- 5. Future Implications and Research Directions
- 6. Understanding Diabetes: A Growing Global Concern
- 7. Frequently Asked Questions About the Breath Sensor
- 8. Could this breath test differentiate between type 1 and type 2 diabetes based on VOC profiles?
- 9. Quick Diabetes Detection: Revolutionize Screening with New Breath Test Developed to identify condition in Minutes
- 10. The Dawn of Non-Invasive Diabetes Screening
- 11. How Does the Diabetes Breath Test Work?
- 12. Benefits of Breath-Based Diabetes Diagnosis
- 13. Understanding the Different Types of Diabetes & the Role of Early Detection
- 14. Real-World Applications and Current Research
- 15. Practical Tips for Diabetes Prevention and Management
University Park, PA – A groundbreaking new sensor developed by a team at Penn State University could revolutionize how diabetes is detected and managed.The device, which analyzes a person’s breath for elevated acetone levels, offers a fast, non-invasive choice to customary diagnostic methods.This breakthrough arrives as nearly one in five of the 37 million adults in the United States living with diabetes remain unaware of their condition, according to recent data from the Centers for Disease Control and Prevention.
The Science Behind the Breath Test
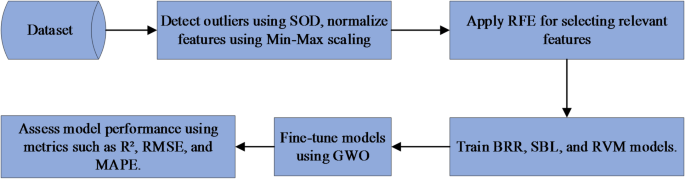
Led by huanyu “larry” Cheng, a Professor of Engineering Science and Mechanics at Penn State, researchers have created a sensor capable of diagnosing both diabetes and prediabetes within minutes. Their findings, recently published in Chemical Engineering Journal, highlight the potential of acetone as a key biomarker for the disease. While acetone is a natural byproduct of fat metabolism, considerably higher concentrations – above approximately 1.8 parts per million – strongly suggest the presence of diabetes.
“Existing methods for diagnosing diabetes often require clinic visits and laboratory tests, which can be expensive and time-consuming,” explained Cheng. “Our sensor simplifies the process, requiring only a breath sample for results.” The team’s innovation builds upon previous breath-analysis attempts by focusing on a biomarker that allows for immediate, on-site detection, rather than needing further laboratory confirmation.
Laser-Induced Graphene: A Key Component
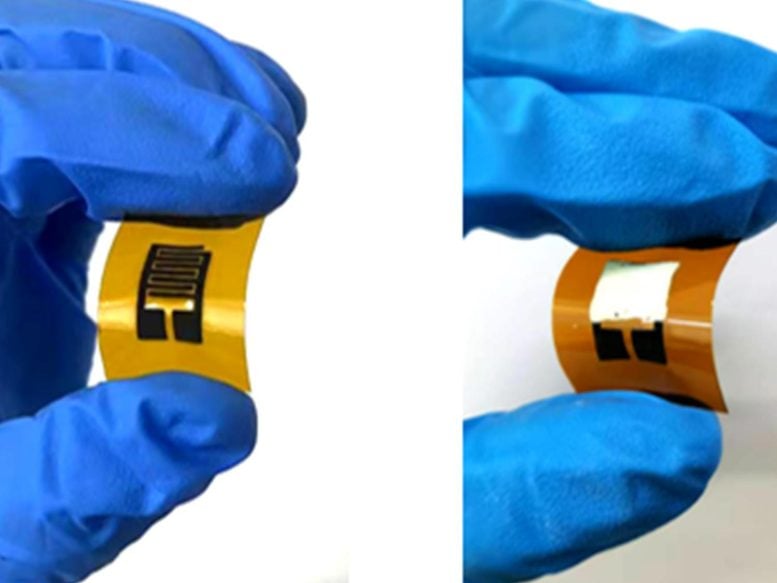
The sensor’s effectiveness hinges on the use of laser-induced graphene, a material produced by exposing a carbon-based substrate to a CO₂ laser. This process creates a patterned, porous graphene structure with unique sensing capabilities.
“The process is akin to toasting bread to carbon black if it’s toasted for too long,” Cheng stated. “By carefully controlling the laser’s power and speed, we can transform the substrate into a few-layered, porous graphene form.”
Overcoming Technical Hurdles
To achieve accurate and selective detection, the researchers combined the laser-induced graphene with zinc oxide.This combination created a junction that enhanced the sensor’s ability to distinguish acetone from other gases.A crucial challenge also involved addressing the potential interference of water molecules in breath. To solve this, the team introduced a selective membrane that blocked water while allowing acetone to pass through.
Currently, the sensor requires users to exhale directly into a bag. Future development aims to refine the technology for direct nose application or integration into a mask, leveraging the condensation within exhaled breath for detection.
Future Implications and Research Directions
Cheng envisions expanding the sensor’s capabilities beyond diagnosis. “If we can understand how acetone levels in breath fluctuate with diet and exercise, similar to how glucose levels respond to food intake, it would unlock exciting opportunities for personalized health management,” he stated. This could pave the way for optimizing health initiatives and empowering individuals to proactively manage their well-being.
| Feature | Traditional Methods | Breath Sensor |
|---|---|---|
| Time to Result | Hours to Days | Minutes |
| Invasiveness | Invasive (blood draw) or minimally invasive (sweat test) | Non-invasive |
| Cost | Generally higher | Potentially lower |
| Convenience | Requires clinic visit | Can be used at home or point-of-care |
Understanding Diabetes: A Growing Global Concern
Diabetes is a chronic metabolic disease characterized by elevated blood sugar levels. According to the World Health Organization, the number of people with diabetes has risen dramatically over the past four decades, from 108 million in 1980 to 422 million in 2014. It is a leading cause of blindness, kidney failure, heart disease, and stroke. Early diagnosis and effective management are crucial to preventing these complications.
There are several types of diabetes including Type 1, Type 2, Gestational Diabetes and others. Type 2 diabetes, which accounts for the vast majority of cases, is often linked to lifestyle factors such as obesity, physical inactivity, and unhealthy diet.
Frequently Asked Questions About the Breath Sensor
- What is the key principle behind the diabetes breath sensor? The sensor detects elevated levels of acetone in exhaled breath, a strong indicator of diabetes.
- How accurate is this breath sensor compared to traditional diabetes tests? Early results show promise, but more research is still underway to determine the sensor’s accuracy.
- Will this sensor eventually replace current diabetes testing methods? It has the potential to become a valuable screening tool and supplement traditional methods, but full replacement is not yet certain.
- How dose laser-induced graphene contribute to the sensor’s effectiveness? The porous nature of laser-induced graphene enhances gas capture and its combination with zinc oxide improves selectivity.
- What are the next steps in the development of this technology? Researchers are working to refine the sensor for direct nose application or mask integration, and to explore potential applications beyond diagnosis.
What are your thoughts on the potential of breath-based diagnostics? Do you think this technology could make diabetes screening more accessible? Share your opinions in the comments below!
Could this breath test differentiate between type 1 and type 2 diabetes based on VOC profiles?
Quick Diabetes Detection: Revolutionize Screening with New Breath Test Developed to identify condition in Minutes
The Dawn of Non-Invasive Diabetes Screening
For decades, diagnosing diabetes mellitus has relied on blood tests – a process that can be inconvenient, sometimes painful, and often delays timely intervention. Now, a groundbreaking new breath test for diabetes is poised to revolutionize diabetes screening, offering a quick, non-invasive, and potentially life-saving method for identifying the condition in mere minutes. This innovation addresses a critical need, considering the rising global prevalence of type 1 diabetes, type 2 diabetes, and gestational diabetes.
How Does the Diabetes Breath Test Work?
The science behind this new diabetes detection method centers on identifying volatile organic compounds (VOCs) present in exhaled breath. Individuals with diabetes exhibit a unique VOC profile due to metabolic alterations caused by insufficient insulin or insulin resistance.
HereS a breakdown of the process:
- Breath Collection: Patients simply breathe into a specialized device.
- VOC Analysis: The device utilizes advanced sensor technology – frequently enough nanomaterial-based sensors or gas chromatography-mass spectrometry (GC-MS) – to analyze the breath sample.
- Data Interpretation: sophisticated algorithms compare the VOC profile to established patterns associated with diabetes symptoms and blood glucose levels.
- Rapid results: A diagnosis, or indication for further testing, is available within minutes.
This contrasts sharply with conventional methods like the A1C test, fasting plasma glucose (FPG) test, and oral glucose tolerance test (OGTT), which require blood draws and laboratory analysis, frequently enough taking hours or days for results.
Benefits of Breath-Based Diabetes Diagnosis
The advantages of this new diabetes test are numerous:
* Non-Invasive: Eliminates the need for needles, reducing patient discomfort and anxiety.
* Rapid Results: Enables quicker diagnosis and initiation of diabetes treatment.
* Cost-Effective: Potentially lower costs compared to traditional blood tests, especially for large-scale diabetes screening programs.
* Increased accessibility: Can be deployed in various settings, including primary care clinics, pharmacies, and even remote locations.
* Early Detection: Facilitates early identification of prediabetes and diabetes, allowing for proactive lifestyle changes and preventative measures.
* Improved patient Compliance: The ease of the test encourages more people to get screened, leading to better diabetes management.
Understanding the Different Types of Diabetes & the Role of Early Detection
early and accurate diabetes diagnosis is crucial because the condition can silently damage organs over time. Here’s a quick overview of the main types:
* Type 1 diabetes: An autoimmune condition where the body attacks insulin-producing cells in the pancreas. Frequently enough diagnosed in childhood or adolescence.
* Type 2 Diabetes: Characterized by insulin resistance and progressive loss of insulin secretion. Strongly linked to lifestyle factors like obesity and inactivity.
* Gestational Diabetes: Develops during pregnancy and can led to complications for both mother and baby.
* Prediabetes: Elevated blood sugar levels that are not high enough to be diagnosed as diabetes, but indicate an increased risk of developing the condition.
The breath test shows promise in differentiating between these types, potentially aiding in personalized diabetes care.
Real-World Applications and Current Research
Several research groups worldwide are actively developing and refining diabetes breath tests.
* clinical Trials: Ongoing clinical trials are evaluating the accuracy and reliability of different breath test prototypes. Initial results have shown promising sensitivity and specificity, comparable to some traditional blood tests.
* Point-of-Care Diagnostics: Companies are working to create portable, user-amiable devices for point-of-care diabetes testing.
* Mass Screening Programs: Public health organizations are exploring the potential of using breath tests for large-scale diabetes screening in high-risk populations.
Such as, a study published in [insert relevant journal/publication if available – replace this bracketed text] demonstrated the feasibility of using a breath test to identify individuals with undiagnosed type 2 diabetes in a community setting.
Practical Tips for Diabetes Prevention and Management
While the breath test offers a revolutionary screening tool, proactive lifestyle choices remain paramount in preventing and managing diabetes:
* Maintain a Healthy Weight: Achieve and maintain a healthy body mass index (BMI).
* Eat a Balanced Diet: Focus on whole foods, fruits, vegetables, and lean protein. Limit processed foods, sugary drinks, and saturated fats.
* Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise per week.
* Regular Checkups: Undergo routine medical checkups, including blood glucose testing, as recommended by your healthcare provider.
*