Japan Takes a Bold Step: Over-the-Counter Emergency Contraception and What It Means for the Future
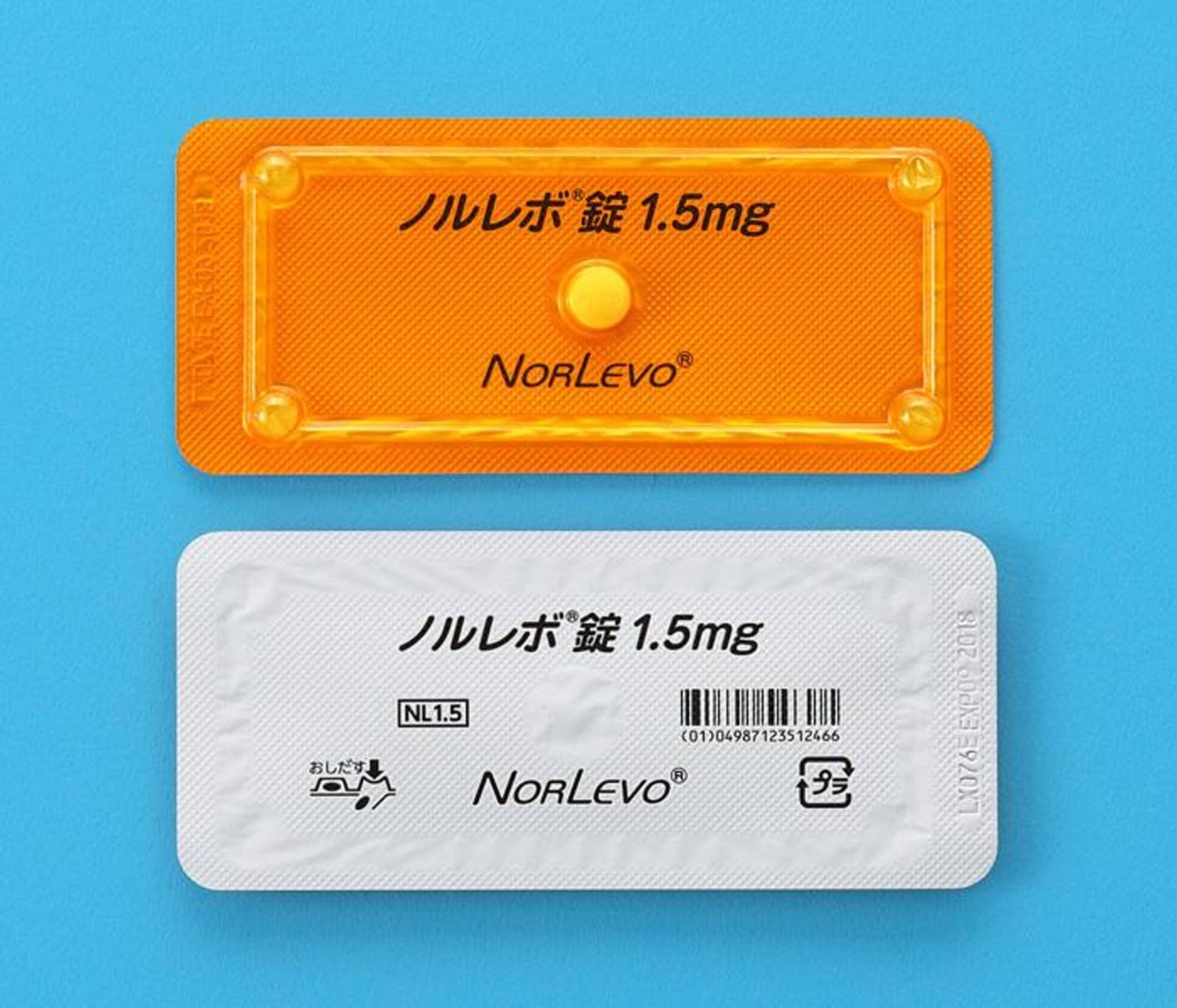
For decades, access to emergency contraception in Japan required a doctor’s visit. Now, that’s changing. The health ministry’s approval of Aska Pharmaceutical’s Norlevo for over-the-counter (OTC) sale marks a seismic shift in reproductive healthcare access – and a potential bellwether for similar changes across Asia. This isn’t just about convenience; it’s about empowering individuals and reshaping conversations around sexual health.
A Landmark Decision: Breaking Down the Details
The move, announced Monday, makes Japan the first country in Asia to allow the sale of an emergency contraceptive pill without a prescription. Norlevo, effective in preventing unwanted pregnancy in approximately 80% of cases when taken within 72 hours of intercourse, will be available as early as this fiscal year. Crucially, there will be no age restrictions, nor will parental consent be required. This contrasts sharply with regulations in many other nations, including parts of Europe and the United States, where age limits or prescription requirements remain in place.
However, access won’t be entirely unrestricted. To prioritize safety, purchasers will be required to obtain the medication in front of a trained pharmacist. This consultation aims to ensure proper understanding of the drug’s usage and potential side effects. Aska Pharmaceutical initially applied for OTC approval in June 2024, and the Ministry panel’s agreement in August paved the way for this historic decision.
Beyond Access: The Wider Implications for Women’s Health
The approval of **emergency contraception** isn’t simply about providing another option; it’s about addressing systemic barriers to reproductive healthcare. For many, the previous requirement for a doctor’s appointment presented significant hurdles – time constraints, financial costs, and geographical limitations all played a role. Removing these obstacles is expected to disproportionately benefit women in rural areas and those with limited access to healthcare facilities.
This change also has the potential to reduce the rate of unintended pregnancies. While comprehensive sex education and readily available contraception are vital, emergency contraception serves as a crucial safety net. According to the Guttmacher Institute, unintended pregnancies still account for a significant percentage of all pregnancies globally, highlighting the ongoing need for accessible options.
The Pharmacist’s Role: A New Frontier in Healthcare
The requirement for pharmacist consultation is a key element of this new system. It places a greater responsibility on pharmacists to provide accurate information and counseling regarding emergency contraception. This could lead to increased training and specialization for pharmacists in reproductive health, potentially expanding their role in preventative care. This model – requiring consultation but not a prescription – could become a template for other countries considering similar reforms.
Looking Ahead: Regional Trends and Potential Challenges
Japan’s decision is likely to spark debate and discussion across Asia. Countries with more conservative social norms may face greater resistance to similar changes. However, the growing global movement towards greater reproductive autonomy suggests that Japan’s move could be the first of many. We can anticipate increased pressure on governments throughout the region to re-evaluate their own regulations regarding emergency contraception.
One potential challenge lies in addressing misinformation and stigma surrounding emergency contraception. Public education campaigns will be crucial to dispel myths and ensure that individuals have access to accurate information. Furthermore, ensuring equitable access for all women, regardless of socioeconomic status or geographical location, will be paramount.
The future of reproductive healthcare in Japan – and potentially across Asia – is being reshaped. This isn’t just about a pill; it’s about empowering individuals, promoting responsible sexual health, and fostering a more equitable healthcare system. What impact will this have on family planning rates and public health initiatives in the coming years? Share your thoughts in the comments below!