Glioblastoma Research: A Turning Point as “Death Sentence” Diagnosis Faces New Hope
Imagine a future where a glioblastoma diagnosis isn’t a period at the end of a life story, but a challenging chapter demanding aggressive, personalized treatment. For Anne McEntee, whose husband Tom lost his battle with this aggressive brain tumor in 2015, that future isn’t just a dream – it’s a necessity fueled by ongoing research and a refusal to accept the status quo. Her tireless fundraising, exceeding £37,000 for Brain Tumour Research, underscores a growing movement: the belief that glioblastoma, while formidable, doesn’t have to be a death sentence.
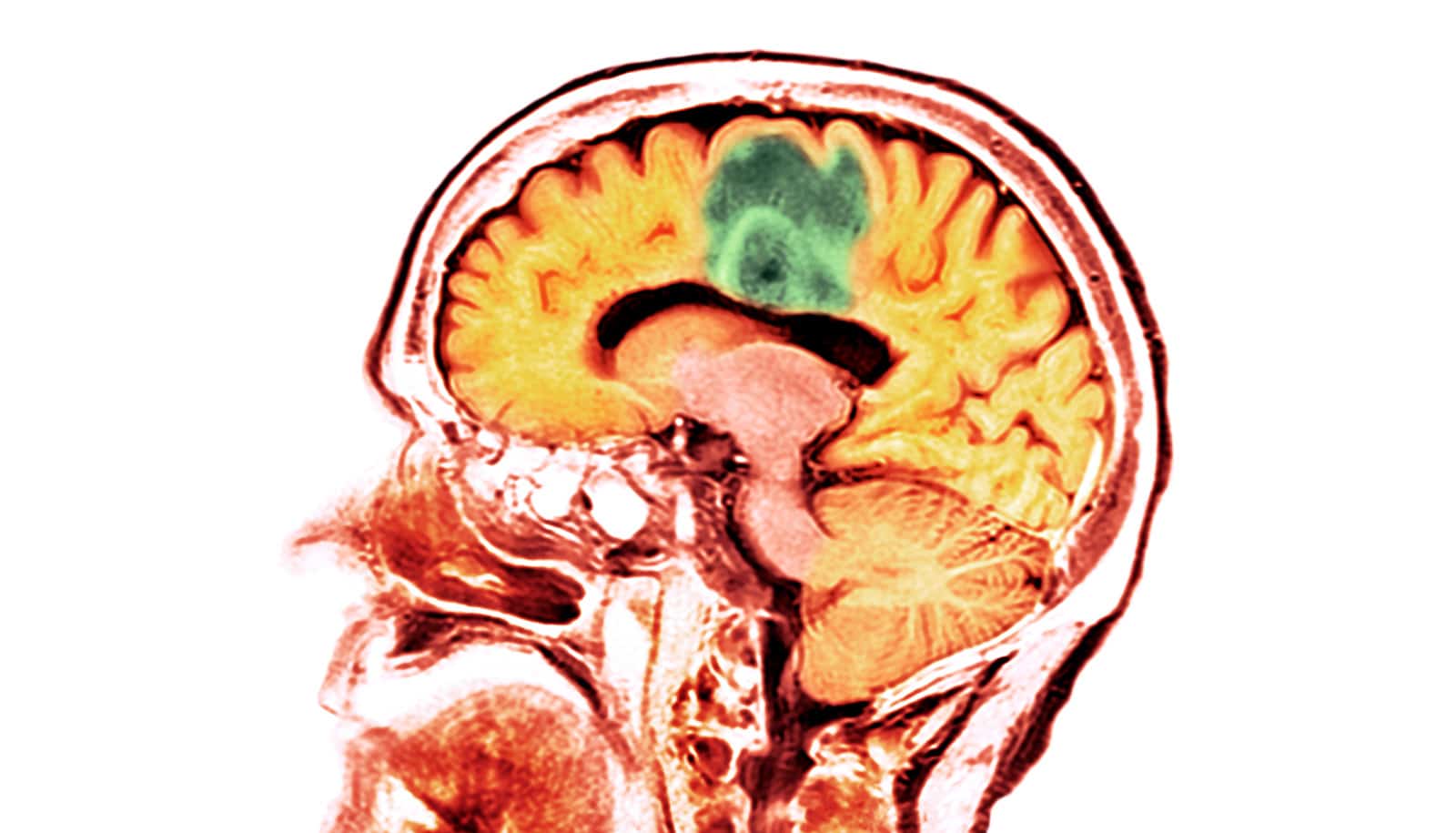
The Harsh Reality of Glioblastoma Today
Glioblastoma, the most common and aggressive type of brain tumor in adults, presents a uniquely difficult challenge. Its rapid growth, infiltrative nature, and resistance to conventional treatments contribute to a median survival rate of just 15-18 months after diagnosis. The McEntee family’s experience – witnessing Tom’s swift decline from a vibrant, active grandfather to someone struggling with debilitating side effects from chemotherapy, radiotherapy, and multiple surgeries – is tragically common. The physical toll, including significant weight gain from steroids and eventual vision loss, highlights the devastating impact of both the disease and its treatment.
“We didn’t have a clue what a glioblastoma was, but we soon discovered it was a death sentence for Tom,” Ms. McEntee shared, a sentiment echoing the shock and helplessness felt by countless families. But within that despair lies a powerful catalyst for change.
Personalized Medicine: The Frontier of Glioblastoma Treatment
The key to shifting the narrative around glioblastoma lies in moving beyond a “one-size-fits-all” approach to treatment. Glioblastoma is not a single disease; it’s a spectrum of genetically distinct tumors. This realization is driving the development of personalized medicine strategies, tailoring treatment plans to the unique molecular profile of each patient’s tumor.
Research at institutions like Queen Mary University of London, partially funded by Ms. McEntee’s fundraising efforts, is focused on identifying specific genetic mutations within glioblastoma cells. This allows researchers to develop targeted therapies that specifically attack these vulnerabilities, minimizing harm to healthy tissue. Furthermore, gentler therapies for childhood brain tumors are also being explored, recognizing the unique challenges faced by young patients.
Pro Tip: If you or a loved one is diagnosed with glioblastoma, ask your oncologist about genetic testing of the tumor. Understanding the specific mutations present can open doors to clinical trials and personalized treatment options.
The Role of Immunotherapy
Immunotherapy, harnessing the power of the body’s own immune system to fight cancer, is showing promising results in other cancers and is now being investigated for glioblastoma. While challenges remain – glioblastoma cells often suppress the immune response – researchers are exploring strategies to overcome these barriers, including checkpoint inhibitors and adoptive cell therapies. These approaches aim to “wake up” the immune system and enable it to recognize and destroy tumor cells.
Beyond Treatment: Early Detection and Prevention
While advancements in treatment are crucial, the ultimate goal is to prevent glioblastoma from developing in the first place. However, the causes of most glioblastomas remain unknown, making prevention difficult. Research is ongoing to identify potential risk factors, including genetic predispositions and environmental exposures.
Early detection, though challenging due to the often vague initial symptoms of glioblastoma (headaches, seizures, personality changes), is also critical. Increased awareness of these symptoms and prompt medical evaluation can lead to earlier diagnosis and potentially more effective treatment.
Expert Insight: “The biggest hurdle in glioblastoma research isn’t necessarily a lack of ideas, but a lack of sustained funding,” says Dr. Sarah Jones, a neuro-oncologist at the National Cancer Institute. “Consistent investment is essential to translate promising laboratory findings into tangible benefits for patients.”
The Future Landscape: Liquid Biopsies and AI-Powered Diagnostics
Looking ahead, several emerging technologies hold immense potential for transforming glioblastoma care. Liquid biopsies, analyzing circulating tumor DNA in blood samples, offer a non-invasive way to monitor treatment response and detect recurrence. This could revolutionize how glioblastoma is managed, allowing for real-time adjustments to therapy based on the tumor’s evolving genetic profile.
Artificial intelligence (AI) is also playing an increasingly important role. AI algorithms can analyze vast amounts of medical imaging data to identify subtle patterns indicative of early-stage glioblastoma, potentially leading to earlier diagnosis. AI can also assist in predicting treatment response and identifying patients who are most likely to benefit from specific therapies.
Did you know? The blood-brain barrier, a protective mechanism that prevents many drugs from reaching the brain, is a major obstacle in glioblastoma treatment. Researchers are developing innovative strategies to overcome this barrier, including nanoparticles and focused ultrasound.
Frequently Asked Questions
Q: What are the common symptoms of glioblastoma?
A: Common symptoms include persistent headaches, seizures, personality changes, weakness on one side of the body, and speech difficulties. However, these symptoms can also be caused by other conditions, so it’s important to consult a doctor for proper diagnosis.
Q: Is there a cure for glioblastoma?
A: Currently, there is no cure for glioblastoma. However, ongoing research is focused on developing more effective treatments and improving survival rates.
Q: How can I support glioblastoma research?
A: You can support organizations like Brain Tumour Research through donations, fundraising, and volunteering. Raising awareness about the disease is also crucial.
Q: What is personalized medicine in the context of glioblastoma?
A: Personalized medicine involves tailoring treatment plans to the unique genetic profile of each patient’s tumor. This allows for more targeted and effective therapies.
Anne McEntee’s story is a testament to the power of hope, resilience, and the unwavering pursuit of scientific advancement. While the fight against glioblastoma is far from over, the convergence of personalized medicine, immunotherapy, and emerging technologies offers a glimmer of hope for a future where this devastating diagnosis no longer equates to a death sentence. What are your thoughts on the future of brain tumor research? Share your perspective in the comments below!