Summary of the Research on “Chemobrain”
Table of Contents
- 1. Summary of the Research on “Chemobrain”
- 2. What are the common cognitive symptoms experienced by patients undergoing chemotherapy, often referred to as “chemo brain”?
- 3. Chemotherapy and Brain Shrinkage in Breast Cancer Patients
- 4. What is “chemo Brain”?
- 5. How Chemotherapy Impacts the Brain
- 6. Evidence of brain Shrinkage in Breast Cancer Survivors
- 7. Common Cognitive Symptoms Experienced by Patients
- 8. Factors Influencing the Risk of Cognitive Impairment
This article discusses a study investigating “chemobrain,” the cognitive difficulties some cancer patients experience after chemotherapy. Here’s a breakdown of the key findings, limitations, and future directions:
key Findings:
Brain shrinkage: The study found statistically significant (p < .05) reductions in overall brain volume in patients reporting "chemobrain" compared to a control group. This shrinkage overlapped with patterns seen in Alzheimer's disease and vascular cognitive impairment.
Cognitive Impairment: Neurocognitive testing revealed substantially reduced semantic and verbal fluency, and lower scores on the Mini-Mental State Examination in the “chemobrain” group.
Importance Despite Control Group Age: The fact that the control group was older (and therefore naturally prone to some brain atrophy) actually strengthened the significance of the findings, as the chemobrain group showed shrinkage despite the age difference.Vital Caveats & Limitations:
Small Sample Size: The researchers caution that the small sample size limits the strength of conclusions, notably regarding specific brain regions linked to memory.
Single Time Point: The study only assessed brain volume at one point in time. It doesn’t prove that chemotherapy causes ongoing brain shrinkage.
Selection Bias: The study didn’t image all chemotherapy patients, but specifically selected those with the most significant cognitive complaints. This means the results may not be representative of the average chemotherapy patient.
Comorbidities: The study didn’t rule out the possibility that some patients already had pre-existing conditions like Alzheimer’s disease that contributed to their cognitive issues.
No Cause-and-Effect Established: The study demonstrates a correlation between chemotherapy and brain changes/cognitive impairment, but doesn’t prove a direct causation.
Future Research Directions:
Longitudinal Study: The research team plans to follow patients over time to track brain changes and memory recovery.
Expanded Cancer Types: The study will be expanded to include patients with other types of cancer, in both men and women.
Investigating Drug Specificity: Further research is needed to determine if specific chemotherapy drugs are more strongly linked to cognitive problems.
Understanding Predisposition: Researchers need to investigate whether some patients are already predisposed to cognitive decline and therefore more vulnerable to the effects of chemotherapy.
Comparison Group: future studies should compare chemotherapy patients to a control group who did not receive chemotherapy.
Expert Commentary:
Alzheimer’s Association (Rebecca Edelmayer): The research could potentially shed light on why women are at higher risk for dementia.
* Geriatric Psychiatry (Eric Brown): Highlighted the study’s design flaws (selection bias, lack of control for comorbidities) and emphasized the need for more robust longitudinal studies.
In essence,the study provides preliminary evidence suggesting a link between chemotherapy and changes in brain structure and cognitive function. However, it’s a starting point for further inquiry, and more research is needed to understand the nature of this relationship and its long-term implications.
What are the common cognitive symptoms experienced by patients undergoing chemotherapy, often referred to as “chemo brain”?
Chemotherapy and Brain Shrinkage in Breast Cancer Patients
What is “chemo Brain”?
“Chemo brain,” formally known as chemotherapy-related cognitive impairment (CRCI), is a common side effect experienced by many breast cancer patients undergoing chemotherapy. It’s not a clinical diagnosis, but a descriptive term for a cluster of cognitive difficulties. While often temporary, concerns arise regarding potential long-term effects, including measurable changes in brain structure – specifically, brain shrinkage or volume loss. This article explores the link between chemotherapy, breast cancer, and potential cognitive decline, focusing on the neurological impacts and what patients can do. We’ll cover chemo brain symptoms, cognitive impairment, and brain volume changes.
How Chemotherapy Impacts the Brain
Chemotherapy drugs, while targeting cancer cells, don’t exclusively affect them. They can cross the blood-brain barrier, impacting healthy brain tissue. Several mechanisms are believed to contribute to chemotherapy-induced neurotoxicity:
Inflammation: Chemotherapy triggers an inflammatory response in the brain, disrupting neuronal function.
Oxidative Stress: Chemo agents can increase oxidative stress, damaging brain cells.
Neurotransmitter Disruption: Alterations in neurotransmitter levels (like serotonin, dopamine, and acetylcholine) can affect cognitive processes.
Reduced Neurogenesis: Chemotherapy can suppress the formation of new neurons (neurogenesis) in areas like the hippocampus, crucial for memory.
White Matter Changes: Damage to the myelin sheath surrounding nerve fibers (white matter) can slow down data processing.
These processes can lead to noticeable cognitive dysfunction and, in some cases, detectable brain atrophy.
Evidence of brain Shrinkage in Breast Cancer Survivors
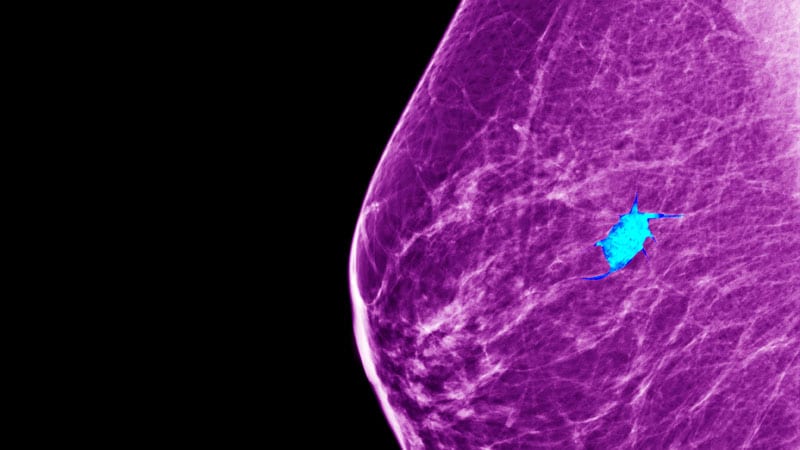
Research using MRI scans has revealed structural brain changes in some breast cancer survivors who received chemotherapy. These changes aren’t universally observed,and their extent varies substantially.
Gray Matter volume: Studies have shown reductions in gray matter volume in areas like the prefrontal cortex (executive function, planning), hippocampus (memory), and temporal lobes (language, memory).
White Matter Integrity: Diffusion tensor imaging (DTI) reveals alterations in white matter integrity, suggesting impaired connectivity between brain regions.
Hippocampal Atrophy: The hippocampus appears especially vulnerable to chemotherapy-induced damage, with some studies demonstrating important shrinkage. This is directly linked to memory problems reported by patients.
Long-Term Effects: While some changes may stabilize or partially reverse after treatment ends, evidence suggests that certain structural alterations can persist for years, perhaps contributing to long-term cognitive impairment.
It’s important to note that these changes aren’t always correlated with the severity of cognitive symptoms. Some individuals with significant brain volume loss may experience mild symptoms, while others with minimal structural changes may have considerable difficulties.
Common Cognitive Symptoms Experienced by Patients
The symptoms of “chemo brain” are diverse and can significantly impact daily life.Common complaints include:
Memory Problems: Difficulty remembering names, dates, or recent events. Short-term memory is often most affected.
Difficulty Concentrating: trouble focusing, easily distracted.
Executive Dysfunction: Challenges with planning, organizing, and problem-solving.
Slowed Processing Speed: Taking longer to process information and respond.
Word-Finding difficulties: Struggling to recall the right words.
Multitasking Challenges: Difficulty handling multiple tasks simultaneously.
Spatial Reasoning Issues: Problems with navigation or understanding spatial relationships.
These symptoms can manifest as difficulties at work, in social situations, or with everyday tasks. Cognitive rehabilitation can be helpful.
Factors Influencing the Risk of Cognitive Impairment
Several factors can influence a patient’s risk of developing chemotherapy-related cognitive impairment and potential brain shrinkage:
Chemotherapy Regimen: Certain chemotherapy drugs (e.g., cyclophosphamide, methotrexate, 5-fluorouracil) are more strongly associated with cognitive side effects. taxol and Adriamycin are also frequently cited.
Dosage and Duration: Higher doses and longer durations of