Breaking: National Assembly to Vet Nutrition and Home-Care Policies Amid Health-Gap Concerns
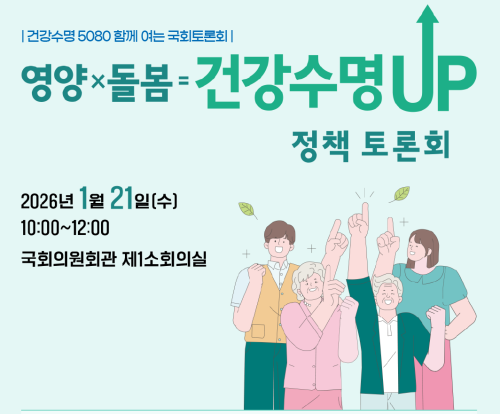
Seoul, Korea — A high-profile policy forum at the National Assembly is poised to examine how nutrition management and care programs can curb a 15-year gap between average life expectancy and healthy life expectancy.
The session is scheduled to begin at 10 a.m. on the 21st, focusing on practical steps to prevent frailty from malnutrition and the worsening of chronic diseases as the life expectancy gap widens.
Officials point to a rising vulnerability among seniors, the chronically ill, and single-person households with disabilities—areas where dietary safety and support services are declining—as key factors behind the shorter healthy lifespan.
Delegates plan to strengthen the public nature of visiting nutrition management services and improve policy linkages that directly reach homes and communities as major agenda items.
The event opens with remarks from National Assembly member Su-jin Lee, followed by welcomes from leaders in nutrition circles, including Jin-seon Song of the Korean Dietitian Association, Dal-rae Joo of the Korean Society of Clinical Nutrition, and Ji-jun Lim of the healthy Lifespan 5080 National Movement Headquarters.
In the session’s second segment, Professor Park So-hyun of Hallym University will discuss “The Meaning and Role of Dietary Management for Extending Healthy Lifespan,” while Professor Lim Hee-sook of Kyung Hee University will address “measures to Link Home Nutritional management Policy to Realize Customized lifelong Care.”
The final panel,chaired by Professor Seung-min Lee of Sungshin Women’s University,will feature experts from academia and government agencies,including Ja-yong Jeong of the Korean Society of Nutrition,Eun-mi Kim of the Korean Society of Clinical Nutrition,Joo-hyeon Lim of the national Institute of Health,Jin-hee Kwon of the National Health insurance Service,and Lim Da-sik from the Ministry of Health and Welfare.
The organizers stated that the debate is expected to become a pivotal platform at the National assembly level for developing field-based nutrition and care response strategies aligned with the national goal of promoting healthy life expectancy.
| Item | Details |
|---|---|
| Healthy vs. Life Expectancy Gap | Average life expectancy: 84.6 years; Healthy life expectancy: 69.3 years; gap ≈ 15 years |
| Date/Time | Session begins at 10:00 a.m. on the 21st |
| Main Focus | Combining nutritional management with care policies to prevent frailty and manage chronic diseases |
| Key Participants | Opening remarks by su-jin Lee; greetings by Jin-seon Song, Dal-rae Joo, Ji-jun Lim; topic presentations by Park So-hyun and Lim Hee-sook; panel chaired by Seung-min Lee |
| Outcome Target | Establish field-based nutrition and care strategies under the Healthy Lifespan initiative |
What this could mean for policy in the months ahead is clear: a coordinated effort to connect home-based nutrition services with lifelong care policies, directly addressing those most at risk in daily life.
Readers: Do you think home-based nutrition support should be a mandatory public service? How should communities balance at-home care with broader health-system resources?
Join the conversation by sharing your views and experiences in the comments below.
>
Data‑Driven Evaluation
Track progress on HALE
Implement the Korean Healthy Ageing Dashboard wiht real‑time metrics on diet quality, functional independence, and hospital readmissions.
Integrated nutrition Strategies
Understanding Korea’s 15‑Year Healthy‑Lifespan Gap
Why the gap matters
- Overall life expectancy in South Korea reached 84.6 years in 2025, while healthy life expectancy (HALE) lagged at 69.2 years – a 15‑year disparity.
- The gap translates into 5.8 million additional years lived with chronic disease, disability, or reduced functional capacity.
- Closing the gap aligns with the “Healthy Korea 2030” vision, which targets a HALE of 75 years by 2030.
Key Drivers Behind the Gap
- Aging Population – 16 % of Koreans were aged 65+ in 2024, projected to rise to 23 % by 2030.
- Nutrition Deficits – High prevalence of malnutrition among older adults (≈ 12 % in community settings, 24 % in long‑term care).
- Fragmented Care – Separate ministries for nutrition (Ministry of Food and Drug Safety) and elder care (Ministry of Health and Welfare) limit coordinated delivery.
- Socio‑economic Inequality – Rural elders experience 30 % higher rates of chronic disease than urban counterparts.
National Assembly Forum: Core Proposals
The National Assembly Forum on Integrated Nutrition and Care (held 18 Nov 2025) presented a three‑track roadmap:
| Track | Objective | Primary Action |
|---|---|---|
| Policy Alignment | Merge nutrition and elder‑care legislation | Draft the Integrated Nutrition‑Care Act (INCA) to create a single governing body. |
| Service Integration | Deliver seamless care across settings | Launch Community‑Based Nutrition‑Care Hubs (cnchs) linking primary clinics, senior centers, and meal‑service providers. |
| Data‑Driven Evaluation | Track progress on HALE | Implement the Korean Healthy Ageing Dashboard with real‑time metrics on diet quality, functional independence, and hospital readmissions. |
Integrated Nutrition Strategies
- standardised Nutrient Screening: Adopt the Mini Nutritional Assessment – Korea (MNA‑K) across all primary health facilities.
- Tailored Meal Programs: Introduce SmartMeal kits that adjust macronutrient ratios based on individual health data (e.g., higher protein for sarcopenia risk).
- Food‑Environment Policy: Incentivise local markets to supply low‑sodium, high‑fiber produce through tax credits and “Healthy Food Zone” zoning.
Care Policy Reforms to Complement Nutrition
- Unified Care Coordination – establish the national Integrated Care Network (NICN) to share electronic health records between hospitals, home‑care agencies, and nutrition services.
- Home‑Based Rehabilitation – Expand the “Aging in Place” program to include physiotherapy visits paired with dietary counselling.
- Workforce Upskilling – Launch a dual‑credential certification for nurses and dietitians focused on geriatric nutrition‑care.
Case Study: Gyeonggi‑do Community Nutrition‑Care Hub
- Pilot launch: July 2024, covering 25 % of the province’s older population.
- Outcomes (2025 data):
- 18 % reduction in hospital admissions for malnutrition‑related complications.
- 12 % increase in the proportion of seniors meeting the Korea Dietary Guidelines for protein intake.
- Participant satisfaction score of 4.7/5 for combined care visits.
benefits of an Integrated Approach
- Health‑economic Gains: Projected ₩4.3 trillion savings in healthcare costs by 2030 through reduced chronic disease burden.
- Improved Quality of Life: Higher scores on the Korean Functional Independence Measure (KFIM) among participants.
- Policy Efficiency: Streamlined budgeting cuts administrative overhead by an estimated 15 %.
Practical Tips for Policymakers and Practitioners
- Start Small, Scale Fast
- Implement pilot CNCHs in high‑need districts, then replicate using the NICN data platform.
- Leverage technology
- Deploy AI‑driven nutrition risk alerts within electronic health records to flag at‑risk seniors during routine visits.
- Engage Stakeholders Early
- Form advisory panels including older adults, caregivers, local farmers, and private meal‑service providers to ensure cultural relevance.
- Monitor Core Metrics Quarterly
- HALE growth rate (target ≥ 0.8 years/yr).
- Nutrition risk prevalence (target ≤ 5 %).
- Readmission rate for preventable conditions (target ≤ 10 %).
International Comparisons: Learning from Neighbours
- Japan: Integrated “Health & Welfare 2025” plan reduced its HALE gap from 12 years (2010) to 8 years (2024) through community meal services and worldwide home‑care.
- Singapore: The “Healthy Ageing Blueprint” pairs mandatory health screenings with subsidised nutrition workshops, achieving a 9‑year gap reduction within a decade.
Future Outlook: 2026‑2030 Roadmap
| Year | milestone |
|---|---|
| 2026 | Enact the Integrated Nutrition‑Care Act; launch the Korean Healthy ageing Dashboard. |
| 2027 | Expand CNCHs to cover 50 % of the elderly population nationwide. |
| 2028 | Achieve a 10‑year reduction in the healthy‑lifespan gap (HALE ≈ 74 years). |
| 2029 | Integrate mental‑health screening into nutrition‑care pathways. |
| 2030 | Meet the “Healthy Korea 2030” target: HALE ≥ 75 years and close the gap to ≤ 9 years. |
key Takeaway
By aligning nutrition policy, elder‑care services, and data analytics under a unified legislative framework, South Korea can transform the 15‑year healthy‑lifespan gap into a measurable public‑health success story—boosting longevity, reducing costs, and enhancing the daily well‑being of millions of seniors.