Cellular Recharge: How Sharing ‘Batteries’ Could Revolutionize Disease Treatment
Imagine a future where doctors don’t just manage the symptoms of debilitating diseases like heart failure or muscular dystrophy, but actually repair the underlying energy deficits driving them. It sounds like science fiction, but a groundbreaking study published in PNAS suggests we’re closer than ever to making that a reality. Researchers at Texas A&M University have discovered a way to boost cells’ natural ability to share mitochondria – the powerhouses of our cells – offering a potential pathway to restore energy where it’s most needed.
The Energy Crisis Within
Mitochondria are essential for life. They convert the food we eat into usable energy, fueling everything from our heartbeat to our thoughts. When these tiny organelles malfunction or are damaged, the consequences can be severe, particularly for energy-hungry organs like the heart, brain, and muscles. Currently, most treatments focus on alleviating symptoms, not addressing the root cause: a lack of cellular energy. But what if we could directly replenish depleted energy stores?
“We’re talking about a fundamental shift in how we approach disease,” explains Dr. Akhilesh Gaharwar, biomedical engineer and lead author of the study. “Instead of just trying to manage the consequences of energy failure, we’re aiming to fix the problem at its source.”
Nanoflowers: Supercharging Cellular Power
Cells naturally share mitochondria, especially when one is under stress. Stem cells are particularly adept at this rescue operation. However, this process is often too limited to be therapeutically effective. The Texas A&M team asked a crucial question: what if we could amplify a cell’s capacity to donate mitochondria?
Their answer lies in molybdenum disulfide (MoS2) nanoflowers – microscopic, flower-shaped particles that act like sponges for harmful reactive oxygen species (ROS). These ROS accumulate during cellular stress and hinder mitochondrial function. By absorbing ROS, the nanoflowers trigger a cascade of events that ultimately leads to increased mitochondrial production.
Key Takeaway: MoS2 nanoflowers don’t directly deliver mitochondria; they enhance the donor cell’s ability to create more mitochondria, making it a more potent energy source for sharing.
In lab tests, stem cells treated with nanoflowers doubled their mitochondrial DNA within just seven days, signaling a significant increase in functional power units. Importantly, this process didn’t require genetic modification or drugs, offering a potentially safer and more accessible therapeutic approach.
Tunneling Nanotubes: The Cellular Delivery System
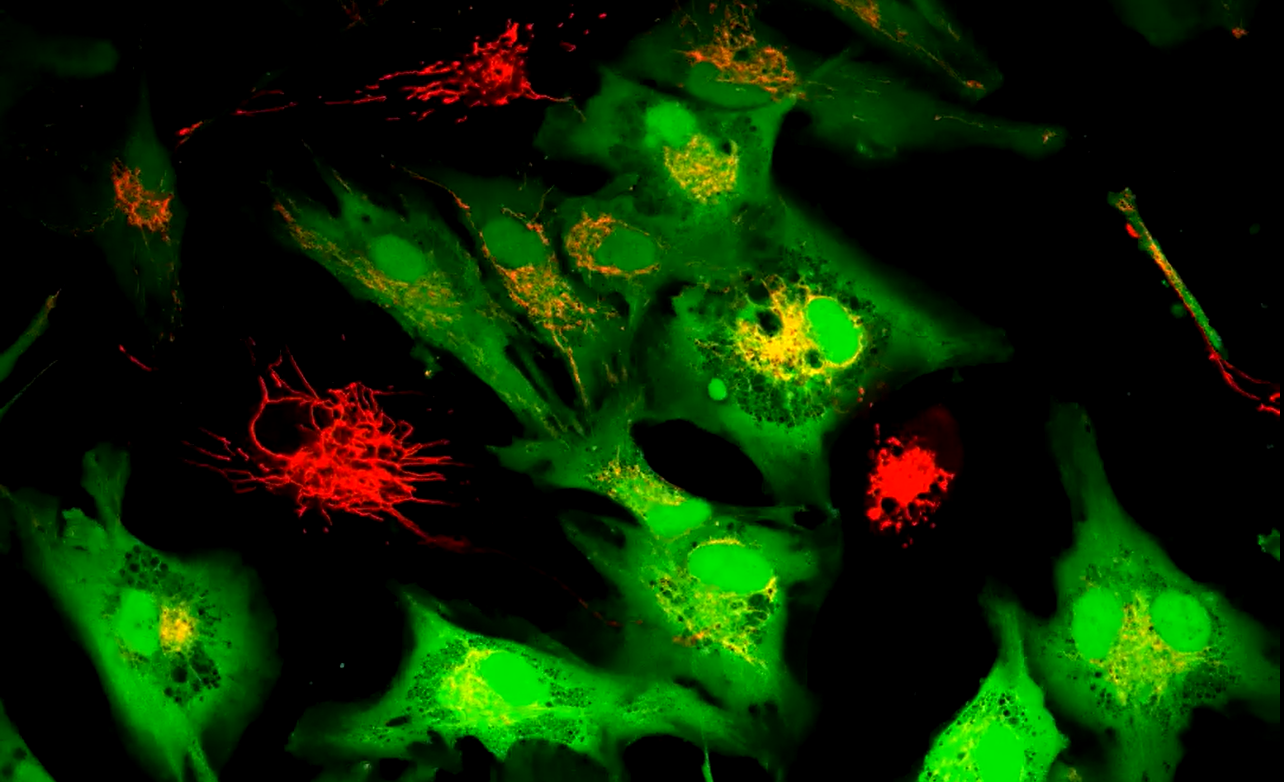
But simply increasing mitochondrial production isn’t enough. The energy needs to get to the cells that need it. Researchers discovered that supercharged stem cells, brimming with mitochondria, could transfer these organelles to damaged cells via microscopic tunnels called tunneling nanotubes.
These nanotubes act as direct conduits, allowing mitochondria to move from healthy donor cells to injured recipient cells. The results were striking: treated stem cells delivered twice as many mitochondria to muscle cells and three to four times more to heart and smooth muscle cells compared to untreated cells. Blocking nanotube formation or physically separating the cells completely halted the transfer, confirming the direct contact mechanism.
Energy Restored: From Lab to Potential Therapies
The transferred mitochondria weren’t just present; they were functional. Measurements showed increased levels of ATP – the cell’s primary energy currency – and heightened oxygen consumption, indicating that the donated organelles were actively generating power. Furthermore, the team observed significant changes in gene expression, with genes involved in energy metabolism and mitochondrial maintenance becoming more active.
To test the therapeutic potential, the researchers exposed cells to toxins known to damage mitochondria. In each case, the donated mitochondria reversed the damage, restoring ATP levels, reducing harmful molecules, and improving cellular health. Heart cells damaged by doxorubicin, a common chemotherapy drug, showed particularly remarkable recovery.
Future Applications: Beyond Symptom Management
The potential applications of this research are vast. From heart disease and muscle disorders to neurodegenerative conditions and even the side effects of cancer treatment, any disease characterized by mitochondrial dysfunction could potentially benefit. Future therapies could involve preparing stem cells with nanoflowers before transplant, or directly targeting weak tissues with the particles.
Researchers are also exploring ways to modify the nanoflowers to target specific organs, such as the brain or heart, for even more precise delivery. However, it’s important to note that this research is still in its early stages. Animal studies are ongoing, and human trials are years away. Safety and efficacy need to be rigorously evaluated before this technology can be widely implemented.
See our guide on stem cell therapy advancements for more information on related research.
The Rise of Mitochondrial Medicine
This research represents a growing trend towards “mitochondrial medicine” – a field focused on restoring and enhancing mitochondrial function to treat disease. Other promising avenues include developing drugs that directly boost mitochondrial biogenesis (the creation of new mitochondria) and identifying genetic factors that contribute to mitochondrial dysfunction.
The convergence of nanotechnology, stem cell biology, and mitochondrial research is creating a powerful synergy, paving the way for a new era of regenerative medicine. The goal is no longer just to manage symptoms, but to fundamentally repair the cellular engines that drive our health.
Frequently Asked Questions
Q: Are MoS2 nanoflowers safe for use in humans?
A: The initial lab tests show the nanoflowers are safe at the tested doses, causing no harm to cell growth or health. However, extensive animal studies and human clinical trials are necessary to confirm their long-term safety and potential side effects.
Q: How long could the benefits of mitochondrial transfer last?
A: That’s a key question researchers are currently investigating. The duration of the benefits will likely depend on factors such as the severity of the initial damage, the efficiency of the transfer process, and the recipient cell’s ability to maintain the newly acquired mitochondria.
Q: Could this technology be used to slow down the aging process?
A: Mitochondrial dysfunction is a hallmark of aging. By restoring mitochondrial function, this technology could potentially slow down some of the effects of aging. However, aging is a complex process with many contributing factors, so this is unlikely to be a complete solution.
Q: What is the difference between mitochondrial biogenesis and mitochondrial transfer?
A: Mitochondrial biogenesis is the process of creating new mitochondria within a cell. Mitochondrial transfer involves the direct movement of existing mitochondria from one cell to another, as demonstrated in this study. Both approaches aim to increase mitochondrial function, but they achieve it through different mechanisms.
What are your thoughts on the potential of cellular energy transfer? Share your comments below!