Cancer Treatment’s Silent Threat: Heart Disease Risk Escalates – Urgent Breaking News
The triumph over cancer is often a long and arduous journey, but a growing body of evidence reveals a hidden cost: a significantly increased risk of heart disease. What was once a concern whispered among oncologists is now a recognized pattern, impacting a rising number of survivors and prompting a new field of medicine – cardio-oncology – to emerge. This is breaking news that demands attention, not just for those currently battling cancer, but for anyone interested in the future of healthcare and long-term wellness. This article is optimized for Google News and SEO to deliver the latest information quickly.
A Problem Decades in the Making
Dr. Bogda Koczwara, a Sydney-based oncologist, first observed this troubling connection in the 1990s. A former police officer, successfully treated for non-Hodgkin lymphoma, returned with worsening health. While the cancer was in remission, tests revealed devastating damage to his heart – silent, permanent damage caused by chemotherapy. This case wasn’t an isolated incident. It was an early warning sign of a phenomenon now affecting millions. Modern cancer therapies, while dramatically improving survival rates, are increasingly recognized as potential contributors to cardiovascular disease.
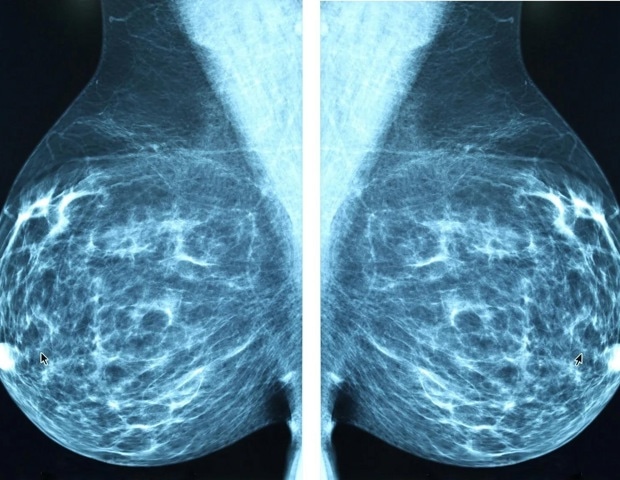
The Rising Tide of Cancer Survivors & Cardiac Complications
The numbers are staggering. Over 18 million cancer survivors in the United States and more than 1.2 million in Australia are living proof of treatment advancements. Europe and Asia are seeing similar increases. But this success comes with a caveat. As patients live longer, they’re experiencing “late effects” – long-term consequences of their treatment, with the cardiovascular system being particularly vulnerable. The very treatments designed to save lives are, in some cases, creating a new health challenge.
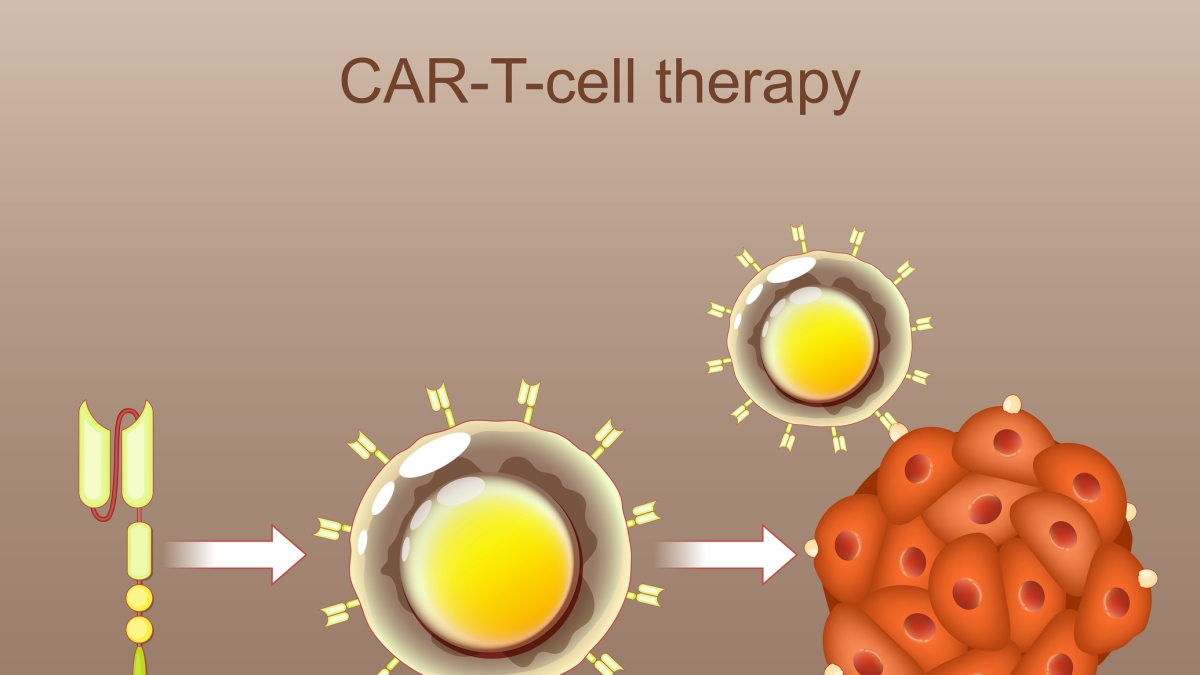
Modern Therapies, Modern Risks
Today’s cancer treatments are far more potent than those available just a few decades ago. Immune checkpoint inhibitors, targeted therapies, and drugs that cut off blood supply to tumors are transforming cancer care. However, these advancements aren’t without risk. Immunotherapies can cause heart inflammation (though rare, it’s life-threatening). Medications affecting blood vessels can elevate blood pressure in up to 40% of patients. Targeted therapies can disrupt essential cardiac functions. And the damage often isn’t immediate; it can take years to manifest, making diagnosis difficult.
Data Confirms the Trend: Heart Disease Deaths on the Rise Among Cancer Survivors
Data from the U.S. Centers for Disease Control and Prevention (CDC) paints a concerning picture. Death certificates listing heart disease as the primary cause, but also indicating a history of cancer, have increased from 4.7 per 100,000 inhabitants in 2019 to 5.5 in 2024. While seemingly modest, experts warn this is an early indicator of a growing problem. Many of these newer oncology medications haven’t been around long enough for their long-term cardiovascular impact to be fully understood.
Cardio-Oncology: A New Field Emerges
Dr. Koczwara, haunted by the fate of his patient, dedicated his career to cancer survivorship and its side effects. He now runs Australia’s first dedicated cancer survivorship center. The medical community is finally responding. Hospitals are establishing specialized cardio-oncology clinics, and researchers are working to identify at-risk patients and develop preventative strategies, including early cardioprotective medication. The cardiac toxicity of anthracyclines, a common chemotherapy drug, was known in the 90s, but the formal field of cardio-oncology was still years away, and the long-term risks weren’t routinely discussed with patients.
Protecting Young Survivors: A Critical Focus
The increasing diagnosis of cancers like leukemia, colorectal cancer, and certain blood cancers in young adults adds another layer of urgency. These survivors face decades of potential cardiovascular risk. Long-term studies show that those who received specific treatments may experience serious heart problems in middle age. Furthermore, pre-existing conditions like obesity, diabetes, and hypertension can amplify the cardiac effects of treatment. Crucially, gaps in follow-up care often occur when patients transition from oncology to primary care.
Virtually all major cancer therapies can leave a mark on the heart, and the effects can be cumulative with multiple treatments. The goal isn’t just cancer remission; it’s ensuring a high quality of life *after* cancer. Cardiovascular risk management is now a central component of post-treatment care, because, increasingly, it’s the heart – not the cancer itself – that will determine a survivor’s long-term well-being.
With information from Bloomberg.
Stay informed with archyde.com for the latest breaking news and in-depth analysis on health, science, and technology. Explore our resources on cancer prevention, heart health, and the evolving landscape of medical care. Don’t miss our upcoming series on proactive health management for cancer survivors – sign up for our newsletter to be notified!