The Emerging Landscape of Neuro-Oncology: Precision Medicine and the Future of Brain Tumor Treatment
Over 185,000 individuals in the U.S. alone are diagnosed with primary and metastatic brain tumors each year, a figure that underscores the urgent need for advancements in treatment. But beyond the sheer numbers, a fundamental shift is underway in how we approach these devastating diseases. A collaborative effort, evidenced by the extensive network of researchers listed – spanning institutions from the University of Toronto to MD Anderson Cancer Center – is driving a move away from generalized protocols towards highly personalized, precision medicine strategies. This isn’t just about incremental improvements; it’s a potential revolution in neuro-oncology, fueled by genomic insights and innovative therapeutic approaches.
Decoding the Genomic Complexity of Brain Tumors
For decades, brain tumors were largely categorized by histological type – glioblastoma, meningioma, etc. However, we now understand that even within these classifications, there’s immense genetic heterogeneity. The work of researchers at UCLA, the University of North Carolina, and institutions across Spain, highlights the critical role of genomic sequencing in identifying specific driver mutations and biomarkers. This isn’t merely academic; it directly impacts treatment decisions. Identifying mutations like IDH1, EGFR, or BRAF allows clinicians to tailor therapies, potentially maximizing efficacy and minimizing side effects.
The increasing sophistication of genomic analysis, including single-cell sequencing, is revealing even more nuanced insights. Researchers are now able to map the evolutionary trajectory of tumors, understanding how they adapt and develop resistance to treatment. This knowledge is crucial for anticipating and overcoming these challenges.
Beyond Surgery and Chemotherapy: Emerging Therapeutic Modalities
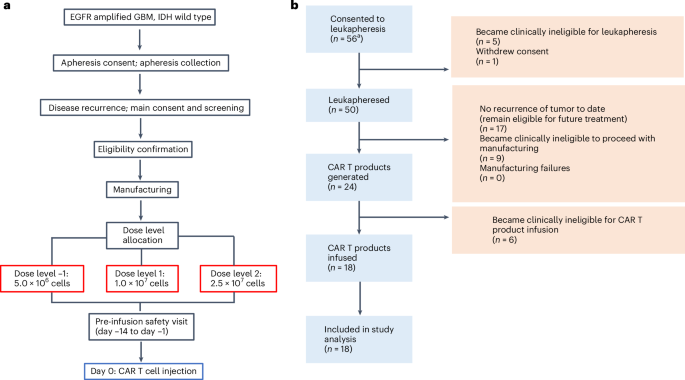
While surgery and chemotherapy remain cornerstones of brain tumor treatment, a wave of novel therapies is gaining momentum. Immunotherapy, once largely unsuccessful in brain tumors due to the immunosuppressive tumor microenvironment, is showing promise with the development of checkpoint inhibitors and CAR-T cell therapies. The involvement of centers like Memorial Sloan Kettering and Northwestern University in these trials is indicative of the growing investment in harnessing the power of the immune system.
The Rise of Targeted Therapies
Targeted therapies, designed to specifically inhibit the activity of mutated proteins, are becoming increasingly prevalent. Drugs targeting BRAF V600E mutations, for example, have demonstrated significant clinical benefit in certain types of brain tumors. Furthermore, research into novel targets, such as KRAS and MYC, is ongoing, offering hope for patients with tumors lacking established therapeutic options. DNATrix Inc.’s involvement signals the growing role of biotechnology companies in developing these cutting-edge treatments.
Viral Therapies and Oncolytic Viruses
A particularly exciting area of research involves oncolytic viruses – genetically engineered viruses that selectively infect and destroy cancer cells. These viruses can also stimulate an immune response against the tumor. The National Cancer Institute’s Laboratory of Pathology is at the forefront of this research, exploring the potential of viral therapies to overcome the challenges of treating aggressive brain tumors.
The Role of Artificial Intelligence and Machine Learning
The sheer volume of data generated by genomic sequencing, imaging studies, and clinical trials is overwhelming. Artificial intelligence (AI) and machine learning (ML) are emerging as essential tools for analyzing this data and identifying patterns that would be impossible for humans to detect. AI algorithms can assist in diagnosis, predict treatment response, and even design new therapies. This is a rapidly evolving field, and its impact on brain tumor treatment is only beginning to be realized.
Addressing the Challenge of the Blood-Brain Barrier
One of the biggest hurdles in treating brain tumors is the blood-brain barrier (BBB), a protective mechanism that prevents many drugs from reaching the tumor. Researchers are exploring various strategies to overcome this barrier, including focused ultrasound, nanoparticles, and the development of drugs that can actively transport across the BBB. The University of Minnesota and the University of Texas MD Anderson Cancer Center are actively involved in these efforts.
The Future of Neuro-Oncology: A Collaborative and Personalized Approach
The future of neuro-oncology isn’t about a single “magic bullet.” It’s about a multifaceted, collaborative approach that integrates genomic sequencing, advanced imaging, immunotherapy, targeted therapies, and AI-driven data analysis. The extensive network of institutions and researchers represented here – from Canada to Spain and across the United States – demonstrates the global commitment to tackling this complex disease. Ultimately, the goal is to move towards a future where pediatric brain tumors and adult gliomas are treated with precision, tailored to the unique characteristics of each patient’s tumor, and offering a significantly improved prognosis. What remains critical is continued investment in research, fostering collaboration, and ensuring equitable access to these innovative therapies.
Explore more insights on precision medicine in oncology in our dedicated section.