The Gut-Brain Axis: How Your Digestive System Impacts Your Mental Health
Table of Contents
- 1. The Gut-Brain Axis: How Your Digestive System Impacts Your Mental Health
- 2. Okay, here’s a breakdown of the key concepts and terms from the provided text, organized for clarity. I’ve categorized them into Gut Health,Mental Health,and the Gut-Brain Connection,and included definitions/explanations based on the text.
- 3. Psychophysiological Connections: Exploring the Interplay Between Mind and Gut Health
- 4. The Gut-brain Axis: A Two-Way Street
- 5. How Mental Health Impacts Gut Health
- 6. How Gut Health Impacts Mental Health
- 7. Dietary Strategies for a Healthy Gut-brain Connection
- 8. Beyond Diet: Lifestyle Factors
- 9. Supplements to Consider (with professional guidance)
- 10. Case Study: The Impact of Dietary Intervention on Anxiety
Graz/Bonn (dpa/tmn) – Ever experience stomach issues when stressed, or feel your mood dip alongside digestive discomfort? You’re not alone. Increasingly, science is revealing a powerful connection between our gut and our brain, known as the gut-brain axis. This isn’t a one-way street; it’s a complex, bi-directional communication network influencing both physical and mental wellbeing.
A Two-Way Conversation
The gut-brain axis describes the intricate interplay between the digestive system and the brain. signals travel in both directions, utilizing the nervous, hormonal, and immune systems – many of which reside within the gut itself. This means what happens in your gut can directly impact your brain, and vice versa.
The Vagus Nerve: A Key Communicator
central to this communication is the vagus nerve, a major component of the parasympathetic nervous system responsible for “rest and digest” functions. A healthy vagus nerve is crucial for relaxation, social interaction, and even recognizing emotions. Emerging research suggests that specific probiotic bacteria, like lactobacilli and bifidobacteria, can positively stimulate the vagus nerve, potentially improving mood and autonomic nerve function over weeks to months.
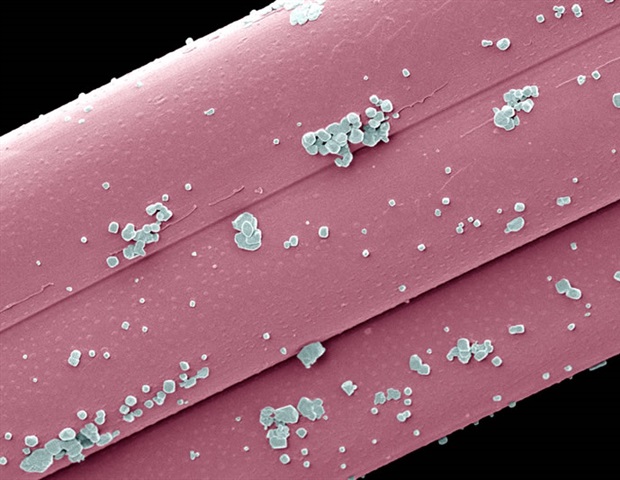
The Microbiome‘s Role: More Than Just Digestion
At the heart of the gut-brain axis lies the microbiome – the trillions of microorganisms inhabiting your intestines. Thes microbes aren’t just aiding digestion; they’re producing vital metabolic products like short-chain fatty acids. These compounds can travel to the brain, delivering signals that impact neurological health. Short-chain fatty acids exhibit anti-inflammatory properties and show promise in managing conditions like Parkinson’s and dementia.
Furthermore,the gut microbiome is a major producer of neurotransmitters,including approximately 90% of the body’s serotonin. While this gut-produced serotonin doesn’t directly enter the brain,it influences psychological processes via the vagus nerve,impacting intestinal movement (too much can cause diarrhea,too little may contribute to depression).
stress,Inflammation,and the Gut-Brain Loop
The connection isn’t just about gut microbes influencing the brain. A stressed brain triggers the release of hormones like adrenaline, which can negatively impact the entire body, including the gut. The immune system also plays a critical role,with proteins called cytokines mediating communication between the gut and brain. Certain gut bacteria promote anti-inflammatory responses, while others can contribute to inflammation linked to anxiety and depression.
Nourishing Your Gut, Nourishing Your Brain
Diet is paramount for cultivating a diverse and healthy gut microbiome. Experts recommend a Mediterranean-style diet rich in:
* Fiber: Found in abundance in fruits, vegetables, and whole grains.
* Fruits & Vegetables: A wide variety of colors provides diverse nutrients.
* Healthy Fats: Olive oil and omega-3 fatty acids from fish are beneficial.
* Fermented Foods: Sauerkraut, kombucha, and kimchi are “synbiotics” – containing both probiotics (live bacteria) and prebiotics (food for the bacteria).
While specific quantities of “superfoods” haven’t been definitively proven, prioritizing diversity in your diet is key.
Ultimately, understanding the gut-brain axis highlights the profound connection between what we eat and how we feel, both physically and mentally.
Okay, here’s a breakdown of the key concepts and terms from the provided text, organized for clarity. I’ve categorized them into Gut Health,Mental Health,and the Gut-Brain Connection,and included definitions/explanations based on the text.
Psychophysiological Connections: Exploring the Interplay Between Mind and Gut Health
The Gut-brain Axis: A Two-Way Street
The connection between our mind and gut health isn’t a new concept, but the depth of this relationship – frequently enough referred to as the gut-brain axis (GBA) – is only now being fully understood. This isn’t a one-way street where the brain dictates gut function; it’s a complex, bidirectional interaction network. Think of it as a constant conversation happening between your brain, the enteric nervous system (frequently enough called the “second brain” located in your gut), and the trillions of gut microbiota residing within your digestive system.
This communication happens through several pathways:
* The Vagus Nerve: This cranial nerve acts as a direct line of communication, transmitting signals in both directions. Vagal nerve stimulation is even being explored as a therapeutic intervention for certain conditions.
* Neurotransmitters: The gut produces a important amount of neurotransmitters, like serotonin (around 90%!), dopamine, and GABA, which directly influence mood, anxiety, and cognitive function. Neurotransmitter imbalance can manifest in both mental and digestive symptoms.
* The Immune System: A large portion of your immune system resides in your gut. Gut inflammation can trigger systemic inflammation, impacting brain function and contributing to conditions like depression and anxiety.
* Short-Chain Fatty Acids (SCFAs): Produced by gut bacteria when they ferment fiber,SCFAs like butyrate,propionate,and acetate nourish gut cells,reduce inflammation,and even influence brain health.SCFA production is directly linked to dietary fiber intake.
* The Endocrine System: The gut influences hormone regulation, including cortisol (the stress hormone), impacting the hypothalamic-pituitary-adrenal (HPA) axis and stress response.
How Mental Health Impacts Gut Health
Stress,anxiety,and depression aren’t just “in your head” – they have tangible effects on your gut. Chronic stress can:
- Alter Gut Microbiota Composition: Stress hormones can reduce the diversity of your gut bacteria, favoring the growth of possibly harmful species. This gut dysbiosis is linked to a range of health problems.
- Increase Gut Permeability (“Leaky Gut”): Stress weakens the tight junctions in your intestinal lining, allowing undigested food particles, toxins, and bacteria to leak into the bloodstream, triggering inflammation. Leaky gut syndrome is a growing area of research.
- Reduce Digestive Function: Stress can slow down digestion, leading to bloating, constipation, or diarrhea. It can also reduce the production of digestive enzymes.
- Exacerbate IBS Symptoms: Individuals with Irritable Bowel Syndrome (IBS) are especially sensitive to the effects of stress on their gut. IBS and mental health are often intertwined.
Real-World Example: During periods of high academic pressure in collage, I observed a significant increase in students presenting with digestive complaints – IBS flare-ups, chronic constipation, and unexplained abdominal pain – directly correlating with reported stress and anxiety levels.
How Gut Health Impacts Mental Health
the influence isn’t just one-way. A compromised gut can significantly impact your mental wellbeing.
* Inflammation & Mood disorders: Chronic gut inflammation can contribute to the progress of mood disorders like depression and anxiety. Inflammation disrupts neurotransmitter function and brain plasticity.
* Nutrient Absorption & Brain Function: A healthy gut is essential for absorbing vital nutrients like B vitamins, magnesium, and zinc, all crucial for optimal brain function. Nutrient deficiencies can exacerbate mental health symptoms.
* Microbiota-Produced Neurotransmitters: as mentioned earlier, gut bacteria produce neurotransmitters that directly influence mood and cognition. An imbalance in gut bacteria can lead to serotonin deficiency or other neurotransmitter imbalances.
* Impact on Cognitive Function: Emerging research suggests that gut health can even impact cognitive function,including memory and learning. Brain fog is often reported by individuals with gut issues.
Dietary Strategies for a Healthy Gut-brain Connection
Diet plays a pivotal role in nurturing both your gut and your mind.
* Fiber-Rich Foods: feed your gut bacteria with plenty of prebiotic fiber from sources like fruits,vegetables,whole grains,and legumes. This promotes SCFA production.
* Fermented Foods: Incorporate probiotic-rich foods like yogurt, kefir, sauerkraut, kimchi, and kombucha to introduce beneficial bacteria into your gut.
* polyphenol-Rich Foods: Foods like berries, dark chocolate, and green tea are rich in polyphenols, which have antioxidant and anti-inflammatory properties that benefit both gut and brain health.
* Limit Processed Foods, Sugar, and Artificial Sweeteners: these can disrupt gut microbiota balance and promote inflammation. Sugar and gut health have a demonstrably negative relationship.
* Hydration: Drinking plenty of water is essential for optimal digestion and gut health.
Beyond Diet: Lifestyle Factors
Optimizing your gut-brain connection extends beyond what you eat.
* Stress Management: Practice stress-reducing techniques like mindfulness, meditation, yoga, or deep breathing exercises.
* Regular Exercise: Physical activity promotes gut motility and can positively influence gut microbiota composition.
* Adequate Sleep: sleep deprivation can disrupt gut microbiota and increase inflammation. Aim for 7-9 hours of quality sleep per night. Sleep and gut health are intrinsically linked.
* Limit Antibiotic Use: Antibiotics can kill both harmful and beneficial bacteria in your gut. Use them only when absolutely necessary and consider probiotic supplementation afterward.
Supplements to Consider (with professional guidance)
while a food-first approach is always best, certain supplements may be beneficial:
* Probiotics: Choose a high-quality probiotic with diverse strains.
* Prebiotics: Consider a prebiotic supplement if you struggle to get enough fiber in your diet.
* L-Glutamine: An amino acid that can help repair the gut lining.
* Omega-3 Fatty Acids: Have anti-inflammatory properties that benefit both gut and brain health.
* Magnesium: Plays a role in stress regulation and gut motility.
Case Study: The Impact of Dietary Intervention on Anxiety
A 2017 study published in BMC Psychiatry followed individuals with diagnosed anxiety disorders who were placed on a modified Mediterranean diet rich in whole foods, fermented foods, and prebiotic fiber for 12 weeks. Researchers observed significant reductions in anxiety symptoms, alongside improvements in gut microbiota diversity and reduced markers of inflammation. This highlights the potential of dietary interventions for anxiety and the crucial role of the gut-brain axis.
disclaimer: This article is for informational purposes only and should not be considered medical advice. always consult with a qualified healthcare professional before making any changes to your diet or treatment plan.