BREAKING: Colonoscopy quality Linked to Survival in Interval cancer Cases
New study reveals surprising outcomes for patients who develop colorectal cancer after screening.
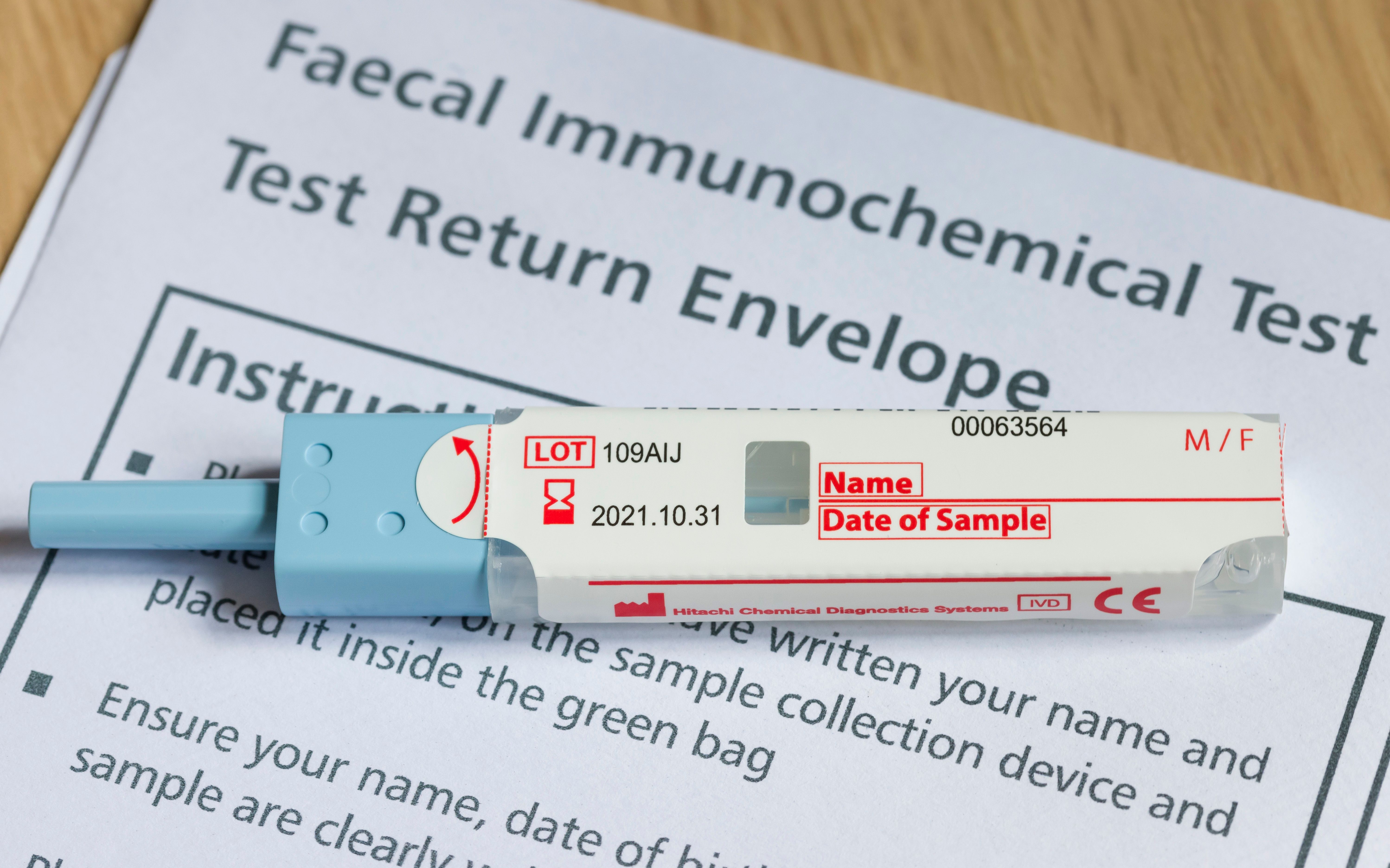
A recent study published in JAMA Network Open has shed light on a complex aspect of colorectal cancer (CRC) screening: interval cancers, those diagnosed after an initial negative screening result. The research found a stark difference in outcomes for patients who developed CRC after a negative fecal immunochemical test (FIT) compared to those diagnosed after a negative colonoscopy following a positive FIT.
The study identified 4,018 cases of interval CRC among 15,386 total CRC diagnoses. A meaningful portion, 2,782 cases (18.1%), occurred after a negative FIT result. Crucially, an additional 1,236 cases (8.1%) were diagnosed following a negative colonoscopy despite a positive FIT result.
Key Findings:
Higher Incidence and mortality After Colonoscopy: The incidence of interval CRC detected after a colonoscopy (0.75 per 1000 person-years) was significantly higher than that detected after a FIT (0.09 per 1000 person-years). This trend was mirrored in CRC-specific mortality, which was also substantially higher in the post-colonoscopy group (0.12 per 1000 person-years) compared to the post-FIT group (0.02 per 1000 person-years). Adjusted hazard ratios (AHRs) confirmed these disparities, showing a 7-fold increase in incidence and a 5-fold increase in mortality for post-colonoscopy interval CRC.
The Paradox of Adenoma Detection Rate (ADR): The study also explored the impact of hospital-level Adenoma Detection Rate (ADR),a measure of how frequently enough adenomas are found during colonoscopies. Surprisingly, higher ADR was associated with a reduction in interval CRC incidence and mortality overall.However, a concerning caveat emerged: among patients who developed interval CRC after a colonoscopy, those in high-ADR settings experienced higher CRC-specific mortality compared to those in low-ADR settings. This suggests that while a higher ADR might indicate better polyp detection, it doesn’t necessarily translate to improved survival in these specific “missed” cancer cases.
Evergreen Insights:
This research offers critical insights into the ongoing efforts to improve colorectal cancer screening and prevention:
Limitations of Current Screening: The findings suggest that even with advanced screening tools like colonoscopy, there are inherent limitations in detecting all precancerous lesions or early-stage cancers. The “ceiling effect” for current colonoscopic techniques and quality assurance, as noted by the researchers, highlights the need for continuous innovation.
The Importance of Both Screening and Quality: While FIT is effective at identifying individuals who need further inquiry, the study underscores that a negative colonoscopy is not an infallible guarantee against future cancer. Meticulous colonoscopy technique and diligent follow-up remain paramount. The paradox of ADR points to a complex interplay of factors,perhaps including patient selection,lesion characteristics,and the skill of the endoscopist,which warrant further investigation.
* Future Directions: The researchers’ call for innovative preventive and therapeutic interventions is timely. Understanding the biological and instrumental factors contributing to interval cancers is crucial for developing strategies that not only detect but also effectively manage these challenging cases, ultimately leading to better patient survival outcomes. As screening technologies evolve, vigilance in identifying and addressing interval cancers will remain a cornerstone of effective CRC control.
What potential reasons explain the “detection paradox” where increased adenoma detection rates correlate with higher colorectal cancer incidence?
Table of Contents
- 1. What potential reasons explain the “detection paradox” where increased adenoma detection rates correlate with higher colorectal cancer incidence?
- 2. Adenoma Detection Boosts CRC Rates, Diminishes Survival
- 3. The Paradox of Polyp detection: Why More Isn’t Always Better
- 4. Understanding Adenomas and Their Progression
- 5. The Rising ADR and CRC Incidence: A Concerning Correlation
- 6. Diminished Survival: Unpacking the Data
- 7. Duodenal Adenomas: A Related Consideration
- 8. Practical Implications for Screening and Surveillance
Adenoma Detection Boosts CRC Rates, Diminishes Survival
The Paradox of Polyp detection: Why More Isn’t Always Better
For years, the medical community has championed increased colonoscopy screening and polyp detection as the cornerstone of colorectal cancer (CRC) prevention. While removing adenomatous polyps undeniably prevents some cancers, emerging data suggests a troubling trend: increased adenoma detection rates (ADR) are correlated with higher CRC incidence and, surprisingly, diminished survival. This isn’t to say screening is ineffective, but rather that we need to refine our understanding of what these findings mean for patient care and cancer risk assessment.
Understanding Adenomas and Their Progression
Colonic adenomas are abnormal growths in the colon lining. they aren’t cancer yet, but they have the potential to become cancerous over time. There are different types:
Tubular adenomas: The most common type, generally with the lowest risk of malignancy.
Villous adenomas: more likely to become cancerous than tubular adenomas.
Tubulovillous adenomas: A mix of the two, with intermediate risk.
Serrated adenomas: Increasingly recognized as a important pathway to CRC, often missed during standard colonoscopy.
The adenoma-carcinoma sequence describes the progression from normal epithelium to adenoma, then to dysplasia, and finally to invasive colorectal cancer. However, this isn’t a linear process.Not all adenomas become cancerous, and the timeframe for progression varies significantly. factors like size, histology (the type of cells), and grade of dysplasia all play a role. Interestingly,even after complete polypectomy,there remains a risk of interval cancer – cancer developing between screenings.
The Rising ADR and CRC Incidence: A Concerning Correlation
Numerous studies have demonstrated a strong correlation between increasing ADR and rising CRC incidence, particularly in the right colon. This phenomenon is often referred to as the “detection paradox.” Several factors may contribute:
- Increased Colonoscopy Volume: More colonoscopies performed mean more polyps will be found,even small,benign ones that wouldn’t have caused harm if left undetected.
- Enhanced Detection Techniques: High-definition colonoscopes and improved bowel planning techniques lead to better visualization and detection of smaller polyps.
- Right Colon Challenges: Polyps in the right colon are often flatter and more arduous to detect than those in the left colon. Increased focus on right-sided colonoscopy may be uncovering more clinically insignificant lesions.
- Lead-Time Bias: Early detection can appear to improve survival, but it may simply be extending the period between diagnosis and death without actually altering the natural course of the disease.
- Length Bias: Screening programs are more likely to detect slower-growing, less aggressive cancers, while aggressive cancers may develop and progress rapidly between screenings.
Diminished Survival: Unpacking the Data
The link between higher ADR and decreased survival is perhaps the most alarming aspect of this trend. While the exact mechanisms are still being investigated, several hypotheses exist:
Overdiagnosis and Overtreatment: Removing small, benign polyps carries a small risk of complications (bleeding, perforation). Overtreatment of these lesions exposes patients to needless risks.
Shift Towards right-Sided Cancers: Right-sided CRC is frequently enough diagnosed at a later stage and has a poorer prognosis than left-sided CRC. If increased ADR is primarily due to detecting more right-sided polyps, it coudl contribute to a decline in overall survival.
Aggressive Cancer Biology: Some researchers suggest that the increasing incidence of CRC may be driven by a shift towards more aggressive cancer subtypes.
Inadequate Follow-up: Patients with multiple adenomas or high-risk features require more frequent and rigorous surveillance, but adherence to these recommendations can be challenging.
While the focus is often on colorectal adenomas, it’s important to note the existence of duodenal adenomas. These are less common but can also be precursors to cancer. According to Pathology Outlines, distinguishing between intra-ampullary and non-ampullary duodenal adenomas is crucial, with intra-ampullary lesions potentially exhibiting pancreatobiliary or intestinal type epithelium.This highlights the importance of accurate pathological assessment in all adenoma cases.
Practical Implications for Screening and Surveillance
Given these findings, what should clinicians and patients do?
Focus on Quality: Prioritize high-quality colonoscopy with thorough bowel preparation and adequate withdrawal time.
Risk Stratification: Tailor surveillance intervals based on individual risk factors, including polyp size, histology, dysplasia grade, family history, and patient age.
Consider Choice Screening Methods: Cologuard (FIT-DNA) and Capsule Endoscopy may offer alternative screening options for certain individuals.
promote Shared Decision-Making: discuss the potential benefits and risks of colonoscopy screening with patients, allowing them to make informed decisions.
* Invest in Research: Further research is needed to understand the underlying