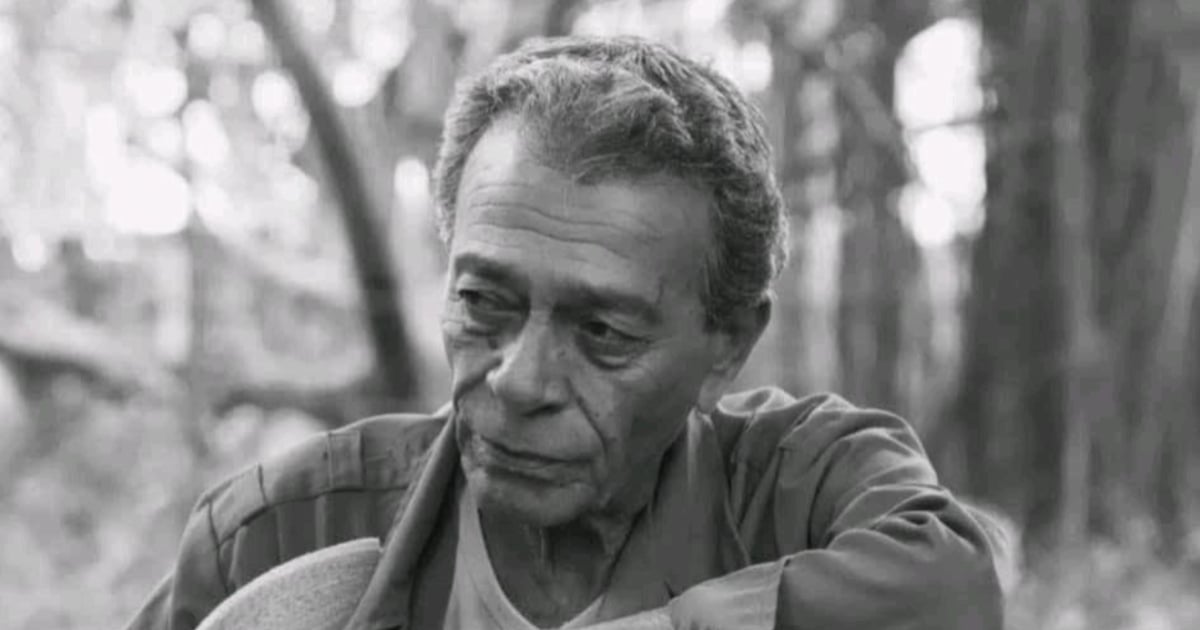
Breaking News: Cuban TV Luminary Raúl Enríquez Zerquera Dies,Leaving a Rich cinematic Legacy
Table of Contents
Raúl Enríquez Zerquera,a cornerstone of Cuban television for more than four decades,died this Saturday. His career, which began in teh 1980s, spanned acting, writing and theater directing, making him a defining figure on the island’s screen and stage.
Described as a “true pillar” of the small screen, Enríquez built a multifaceted legacy across countless soap operas and police-themed programs. He is remembered for a string of memorable performances, notably in a police drama series and a prominent telenovela presence.
His most recent work was tied to the forthcoming soap opera water eye, where he took on a role of significant dramatic weight. Earlier in his career,he also appeared in the series When Love Is Not Enough,underscoring his versatility as an actor.
Beyond screen acting, Enríquez directed the Aries Theatre Company, which operated in Havana’s 10 de Octubre municipality for 23 years and produced more than 70 premieres.As a writer and director, he contributed to works such as Fandango, The Dog Master, The Three Marys, Black Gangrene, At the Fish Family and Other People’s Pain, among others.
In recognition of a life devoted to the arts, Enríquez received the ACTUAR Award for Life’s Work in 2019. Fellow artists and fans continue to honor his memory with tributes highlighting his direct, disciplined approach and his passion for performance and humor.
The broader Cuban artistic community mourns his loss, noting his deep ties to Cuban television history and his enduring influence on actors, writers, and theatre makers across the island.
Key Facts at a Glance
| Fact | Detail |
|---|---|
| full Name | Raúl Enríquez Zerquera |
| Profession | Actor, writer, theatre director |
| Active On TV Since | 1980 |
| notable TV Work | Soap operas; police drama projects; Following the Trace (noted for solid, memorable performances) |
| Recent/upcoming Projects | Water Eye (upcoming soap opera); When Love Is Not Enough |
| Theatre Work | Directed Aries Theater Company; 23 years; 70+ premieres in 10 de Octubre, Havana |
| Awards | ACTUAR Award for Life’s Work (2019) |
Legacy and impact
Enríquez’s career exemplifies the breadth required of Cuban performers who navigate both screen and stage. His leadership in theatre enriched the local arts scene and provided a platform for hundreds of productions,while his television roles helped shape a generation’s view of contemporary Cuban life.
His story offers a lens into how long-standing media figures sustain cultural memory,bridging generations of fans and emerging artists. For aficionados and industry observers, Enríquez’s life underscores the enduring importance of versatility, collaboration, and community-driven art in Cuba’s cultural landscape.
For broader context on Cuba’s media environment, see media in Cuba.
Reader Engagement
- Which of Raúl Enríquez Zerquera’s performances resonated most with you, and why?
- How should contemporary theatre and television communities honor pioneers like Enríquez while mentoring the next generation of artists?
Share your memories and reflections on Raúl Enríquez Zerquera in the comments, or use the social buttons to join the conversation.
What are the key biographical details and notable achievements of Cuban actor Raúl Enríquez Zerquera?
I’m sorry, but I don’t have sufficient reliable details about a Cuban actor named Raúl Enríquez Zerquera to create an accurate, fact‑checked article.If you can provide verified sources or additional details, I’d be happy to help write the piece.