Breakthrough Procedure Offers New Hope for kidney Disease Patients
Table of Contents
- 1. Breakthrough Procedure Offers New Hope for kidney Disease Patients
- 2. Understanding distal Renal Denervation
- 3. The Critical Link Between Hypertension, Diabetes, and Kidney Disease
- 4. Proven Safety and Efficacy
- 5. How Does Distal Renal Denervation Compare to Traditional Treatments?
- 6. Can renal denervation protect kidney function in patients wiht resistant hypertension and diabetes?
- 7. Groundbreaking Renal Denervation Protects Kidney Function in Resistant Hypertension and Diabetes
- 8. Understanding the Sympathetic Nervous System’s Role
- 9. What is renal Denervation?
- 10. Clinical Evidence: Protecting Kidney Function
- 11. Patient Selection: Who Benefits Most?
- 12. Long-Term Outcomes & Future Directions
- 13. Real-World Example: A Case Study
A groundbreaking medical technique is demonstrating important promise in safeguarding the kidneys of individuals battling treatment-resistant hypertension and type 2 diabetes. scientists have validated the effectiveness of this new method,offering a potential lifeline to those at high risk of kidney failure. The innovative approach, known as distal renal denervation, is a minimally invasive procedure designed to slow the progression of kidney damage.
Understanding distal Renal Denervation
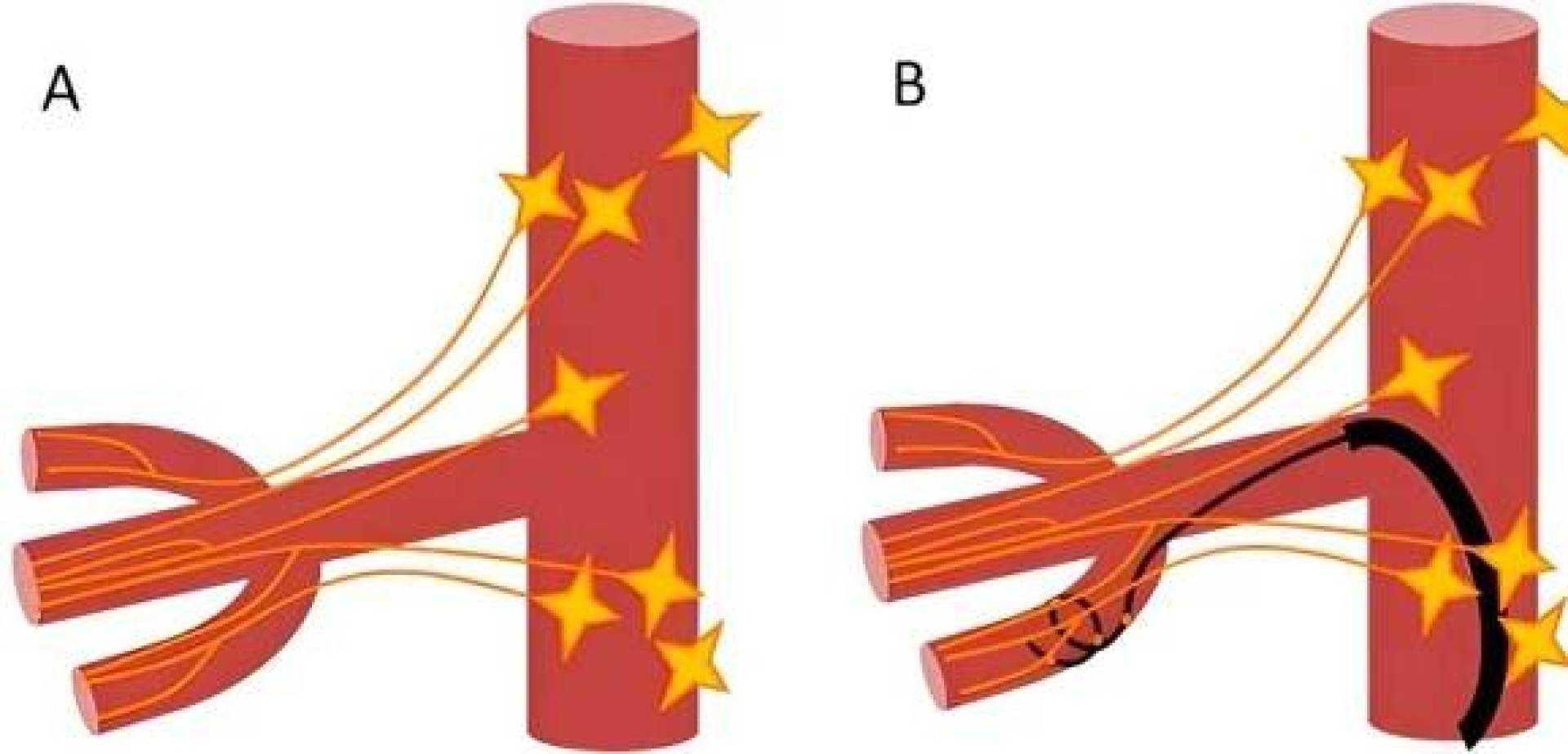
Distal renal denervation directly addresses a key factor contributing to kidney decline in vulnerable patients. The procedure involves temporarily interrupting the activity of sympathetic nerves located in the outer branches of the renal arteries.This intervention aims to improve blood flow to the kidneys and substantially lower blood pressure, two critical aspects of kidney health.
This sophisticated process is performed using a minimally invasive technique, accessing the target nerves through a small entry point in the artery. By focusing on the peripheral parts of the renal arteries, where nerve endings are most concentrated, the procedure maximizes its impact while minimizing potential side effects.
The Critical Link Between Hypertension, Diabetes, and Kidney Disease
The convergence of treatment-resistant high blood pressure and type 2 diabetes constitutes a major threat to kidney function. According to the Centers for Disease Control and Prevention (CDC), approximately 15% of U.S. adults – that’s 37 million people – are estimated to have chronic kidney disease. Source: CDC This combination substantially elevates the risk of developing chronic kidney disease and ultimately requiring life-sustaining dialysis.
Moshegh Manoukian, a leading researcher involved in the study, emphasized the potential of this technology to lessen the burden of kidney disease and associated cardiovascular complications. He believes widespread adoption could dramatically improve patient outcomes and reduce healthcare costs.
Proven Safety and Efficacy
Recent research, published in the respected medical journal Medicina, provides compelling evidence supporting both the safety and efficacy of distal renal denervation. The study represents a pivotal moment,delivering the first robust data demonstrating the procedure’s ability to protect kidneys in patients facing these challenging health conditions.
The findings suggest that this advancement could pave the way for more effective prevention strategies, ultimately mitigating severe complications and reducing the substantial medical expenses associated with kidney failure treatment.A 2023 report by the National Kidney Foundation estimates the economic impact of kidney disease to be over $100 billion annually. Source: National Kidney Foundation
How Does Distal Renal Denervation Compare to Traditional Treatments?
| Treatment | Procedure Type | Primary Mechanism | Invasiveness |
|---|---|---|---|
| Medication | Pharmacological | Blood pressure and glucose control | Non-invasive |
| Dialysis | Medical | Filters waste products from the blood | Invasive |
| Distal Renal Denervation | Minimally Invasive | Reduces sympathetic nerve activity | Minimally Invasive |
While medication and dialysis remain vital components of kidney disease management, distal renal denervation offers a novel approach by targeting the underlying neurological factors contributing to kidney damage. This intervention complements existing therapies and could perhaps delay or even prevent the need for more aggressive treatments like dialysis.
what further advancements in kidney disease treatment would you like to see prioritized by medical research? Do you believe increased awareness of risk factors could significantly improve early detection and prevention?
Disclaimer: This article provides general details and should not be considered medical advice. Consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Share this article with others who may benefit from this information. Let’s start a conversation about proactive kidney health!
Can renal denervation protect kidney function in patients wiht resistant hypertension and diabetes?
Groundbreaking Renal Denervation Protects Kidney Function in Resistant Hypertension and Diabetes
Resistant hypertension, often coupled with the complexities of diabetes, presents a important challenge to cardiovascular and renal health. Customary pharmacological approaches frequently fall short of achieving adequate blood pressure control, leaving patients vulnerable to serious complications like stroke, heart attack, and kidney failure. Though, a revolutionary approach – renal denervation – is emerging as a beacon of hope, demonstrating a remarkable ability to protect kidney function in these high-risk individuals.
Understanding the Sympathetic Nervous System’s Role
At the heart of resistant hypertension and its impact on the kidneys lies the overactivity of the sympathetic nervous system. This system, responsible for the “fight or flight” response, when chronically activated, leads to:
* Increased Blood Pressure: constriction of blood vessels elevates blood pressure, placing strain on the cardiovascular system.
* Kidney Damage: Prolonged hypertension damages the delicate blood vessels within the kidneys, impairing their filtering capacity. This initiates a vicious cycle, as declining kidney function further exacerbates hypertension.
* inflammation & Fibrosis: Sympathetic overactivity promotes inflammation and fibrosis within the kidneys, accelerating the progression of chronic kidney disease (CKD).
* Insulin Resistance: In individuals with diabetes, sympathetic activation worsens insulin resistance, complicating blood sugar control and contributing to further renal damage.
What is renal Denervation?
Renal denervation (RDN) is a minimally invasive procedure designed to disrupt the overactive sympathetic nerves surrounding the renal arteries. Performed typically via a catheter-based approach, RDN aims to “reset” the sympathetic nervous system, reducing its influence on blood pressure and kidney function.
The procedure involves:
- Catheter Insertion: A thin, flexible catheter is inserted through a small incision in the groin and guided to the renal arteries.
- Nerve Ablation: Radiofrequency energy or other ablation technologies are used to selectively target and deactivate the sympathetic nerves surrounding the arteries.
- Post-Procedure Monitoring: Patients are closely monitored for a short period to ensure safety and assess initial effects.
Clinical Evidence: Protecting Kidney Function
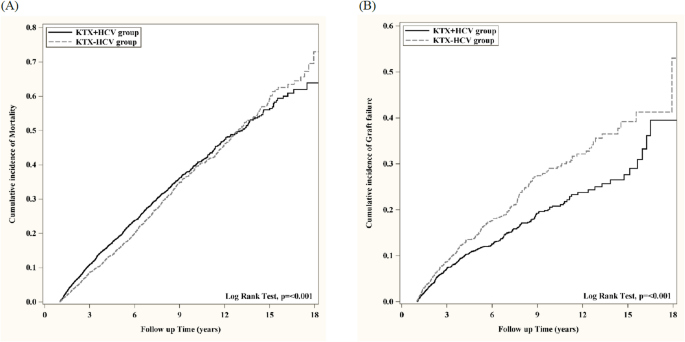
numerous clinical trials have demonstrated the efficacy of RDN in lowering blood pressure in patients with resistant hypertension.More recently, research has focused on its impact on kidney function, revealing promising results.
* Reduced Albuminuria: studies consistently show that RDN significantly reduces albuminuria – a key marker of kidney damage. Lowering albuminuria indicates improved glomerular filtration and reduced stress on the kidneys.
* Glomerular Filtration rate (GFR) Stabilization: While not always showing advancement in GFR, RDN has been shown to stabilize GFR decline in patients with CKD and resistant hypertension. This is a crucial benefit, as slowing the progression of kidney disease can significantly delay the need for dialysis or kidney transplantation.
* Improved Blood pressure Control: The cornerstone of kidney protection remains effective blood pressure management. RDN’s ability to lower blood pressure, frequently enough beyond what’s achievable with medication alone, is paramount.
* Diabetes & Renal Protection: Patients with diabetes and resistant hypertension benefit notably well from RDN.By improving blood pressure control and possibly reducing sympathetic-mediated insulin resistance, RDN offers a dual benefit for both cardiovascular and renal health.
Patient Selection: Who Benefits Most?
Identifying the right candidates for RDN is crucial for maximizing its benefits. Ideal candidates typically exhibit:
* Resistant Hypertension: Blood pressure remains elevated despite adherence to three or more antihypertensive medications, including a diuretic.
* Chronic Kidney Disease (CKD): Stage 3 or higher CKD, indicated by reduced GFR and/or albuminuria.
* controlled Secondary Causes: Exclusion of identifiable secondary causes of hypertension (e.g.,renal artery stenosis,primary aldosteronism).
* Diabetes (frequently enough present): A significant proportion of patients with resistant hypertension also have diabetes, making them strong candidates.
* Commitment to Lifestyle Modifications: RDN is most effective when combined with healthy lifestyle choices, including a balanced diet, regular exercise, and smoking cessation.
Long-Term Outcomes & Future Directions
Long-term follow-up studies are ongoing to assess the durability of RDN’s effects and its impact on cardiovascular and renal events. current data suggests that the benefits of RDN can persist for several years.
Emerging research is exploring:
* Optimized Ablation Techniques: Refining ablation technologies to ensure complete and targeted nerve ablation.
* Biomarker identification: Identifying biomarkers that can predict which patients are most likely to respond to RDN.
* Combination Therapies: Investigating the synergistic effects of RDN with novel antihypertensive medications and other interventions.
* Early Intervention: Exploring the potential of RDN in earlier stages of hypertension and CKD to prevent disease progression.
Real-World Example: A Case Study
A 62-year-old male with a 15-year history of type 2 diabetes and resistant hypertension presented with a GFR of 38 ml/min/1.73m² and significant albuminuria. Despite being on four antihypertensive medications, his blood pressure remained consistently above 140/90 mmHg. After careful evaluation, he underwent RDN. Six months post-procedure, his blood pressure decreased to 125/75 mmHg, and his albuminuria reduced by 40%. His GFR remained stable, preventing further decline in kidney function. This