TAF1: A Crucial Switch for Blood Cell Development Revealed
Table of Contents
- 1. TAF1: A Crucial Switch for Blood Cell Development Revealed
- 2. How might understanding TAF1 inactivation mechanisms lead to the progress of novel epigenetic therapies?
- 3. Unlocking TAF1: A Potential Breakthrough in Cancer Therapy
- 4. What is TAF1 and Why is it Significant?
- 5. The Role of TAF1 in Cancer Development
- 6. Mechanisms of TAF1 Inactivation: A Deeper Dive
- 7. Therapeutic Strategies Targeting TAF1 Deficiency
- 8. Biomarkers and Patient Selection
- 9. Case Studies & Clinical Trials (as of 2024)
Miami, FL – New research is poised to reshape our understanding of how blood cells develop, highlighting a protein named TAF1 as a critical regulator. Findings published in Developmental Cell suggest TAF1 acts as a molecular switch, orchestrating the delicate balance between maintaining blood stem cells and guiding them to mature into specialized blood cells, particularly in adults.
This finding challenges the long-held belief that TAF1 is a worldwide requirement for gene activation in all cells throughout life. Instead, the study indicates TAF1 plays a more nuanced role, specifically promoting gene expression that drives hematopoietic stem cells (HSCs) toward differentiation.”The most surprising discovery is that adult HSCs can survive without an crucial general transcription factor, and that the TAF1 loss only affects the activation of differentiation-associated genes, not the self-renewal-promoting genes,” stated Fan Liu, Ph.D., the study’s lead author and a researcher at Sylvester Thorough Cancer Center.
TAF1’s mechanism of action involves both initiating transcription and releasing a natural brake on the process, according to the research team. This fine-tuned control is vital for healthy blood production.
The implications of these findings are significant, particularly for cancer therapeutics. Developing drugs that effectively target cancer cells without harming normal blood cell production has been a major challenge in hematology. The data suggest that TAF1 inhibitors could be a promising avenue, as inhibiting TAF1 did not impede essential stem cell self-renewal or blood cell production in the study.
“A key question that we needed to address was: if you successfully target TAF1, do you compromise normal blood production? What this paper says is no,” commented Dr. Nimer, a study author.
Furthermore, this research opens doors for improving stem cell transplantation by potentially harnessing TAF1 to enhance the expansion of HSCs in laboratory settings.Future investigations will explore whether TAF1 performs similar regulatory functions in other stem cell populations, such as those found in the colon or brain, and their relevance to cancer.
How might understanding TAF1 inactivation mechanisms lead to the progress of novel epigenetic therapies?
Unlocking TAF1: A Potential Breakthrough in Cancer Therapy
What is TAF1 and Why is it Significant?
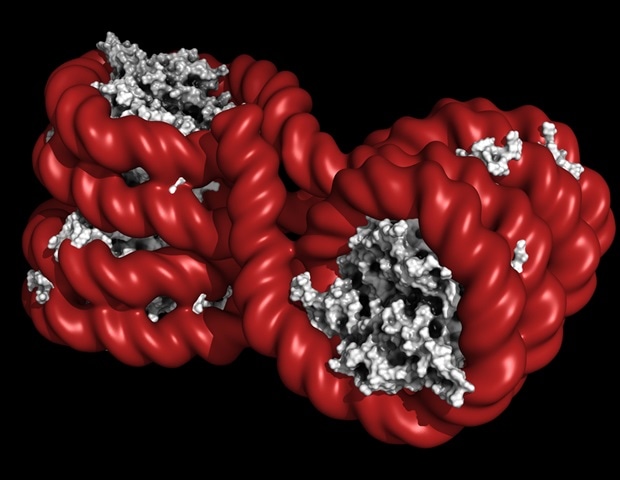
TAF1 (TATA-box binding protein-associated factor 1) is a crucial component of the TFIID complex, a key regulator of gene transcription. Essentially, it helps turn genes “on” or “off.” Recent research, particularly over the last five years, has highlighted TAF1’s frequent inactivation in a wide range of cancers, including ovarian, breast, lung, and hematological malignancies. This inactivation isn’t just a correlation; it’s increasingly understood as a driver of cancer development and progression. Understanding TAF1’s role opens new avenues for targeted cancer therapies. The field of cancer genomics is rapidly advancing our understanding of these genetic drivers.
The Role of TAF1 in Cancer Development
TAF1 acts as a tumor suppressor gene. When it’s functioning correctly, it helps maintain genomic stability and regulates cell growth. However, when TAF1 is mutated or silenced – often through epigenetic mechanisms like promoter methylation – several critical processes are disrupted:
Increased Genomic Instability: Loss of TAF1 leads to errors during DNA replication and repair, accelerating the accumulation of mutations. This is a hallmark of cancer.
Uncontrolled Cell Proliferation: TAF1 normally regulates genes involved in cell cycle control. Its absence allows cells to divide uncontrollably.
Impaired DNA Damage response: cancer cells with TAF1 loss are less able to respond to DNA damage, making them more resistant to conventional therapies like chemotherapy and radiation.
Enhanced Metastasis: Studies suggest TAF1 inactivation can promote the spread of cancer cells to distant sites. Metastatic cancer remains a significant clinical challenge.
Mechanisms of TAF1 Inactivation: A Deeper Dive
TAF1 isn’t typically deleted as a whole gene. Rather, it’s usually inactivated through more subtle mechanisms:
Promoter Methylation: This is the most common mechanism. Adding methyl groups to the TAF1 gene’s promoter region silences its expression. Epigenetic therapy aims to reverse these changes.
Mutations: While less frequent, specific mutations within the TAF1 gene can disrupt its function. These mutations are frequently enough identified through next-generation sequencing (NGS).
MicroRNA Regulation: Certain microRNAs can bind to the TAF1 mRNA, leading to its degradation and reduced protein levels.
Ubiquitin-Proteasome System: Dysregulation of this system can lead to increased degradation of the TAF1 protein.
Therapeutic Strategies Targeting TAF1 Deficiency
The growing understanding of TAF1’s role has spurred the development of several promising therapeutic strategies:
- Epigenetic Modulators: Drugs like 5-azacytidine and decitabine are DNA methyltransferase inhibitors (DNMTis).They can remove methyl groups from the TAF1 promoter, restoring its expression. These are already approved for certain hematological malignancies and are being investigated in solid tumors.
- Synthetic Lethality Approaches: this strategy exploits the fact that cancer cells with TAF1 loss are particularly vulnerable to the inhibition of certain other genes. such as, research suggests that inhibiting certain histone deacetylases (HDACs) can selectively kill TAF1-deficient cells. Synthetic lethality is a hot area of cancer research.
- TAF1 Gene Therapy: While still in early stages, researchers are exploring the possibility of delivering a functional copy of the TAF1 gene directly into cancer cells using viral vectors.
- PARP Inhibitors: TAF1 deficient cancers often exhibit defects in DNA repair pathways. PARP inhibitors, already used in BRCA-mutated cancers, show promise in TAF1-deficient tumors. PARP inhibition is a well-established therapeutic strategy.
- Immunotherapy Combinations: restoring TAF1 expression can enhance the immunogenicity of cancer cells, making them more susceptible to immunotherapy. combining epigenetic modulators with checkpoint inhibitors is an area of active investigation.
Biomarkers and Patient Selection
identifying patients who will benefit from TAF1-targeted therapies is crucial. Several biomarkers are being investigated:
TAF1 mRNA Expression Levels: Low TAF1 mRNA levels, measured through quantitative PCR (qPCR), can indicate TAF1 inactivation.
TAF1 Protein Levels: Immunohistochemistry (IHC) can assess TAF1 protein expression in tumor samples.
Promoter methylation Status: Bisulfite sequencing can determine the methylation status of the TAF1 promoter.
Genomic Sequencing: Identifying mutations within the TAF1 gene through NGS.
Precision oncology relies heavily on identifying these biomarkers to personalize treatment.
Case Studies & Clinical Trials (as of 2024)
While widespread clinical request is still developing,several early-phase clinical trials have shown encouraging results:
Ovarian Cancer: A Phase I trial evaluating decitabine in combination with carboplatin and paclitaxel in patients with recurrent ovarian cancer showed a significant improvement in progression-free survival in patients with TAF1 promoter methylation.
Acute Myeloid Leukemia (AML): Studies have demonstrated that AML patients with TAF1 inactivation are more sensitive to DNMT