New Forest Mouse Species discovered in Sulawesi, Highlighting Indonesian Biodiversity
Table of Contents
- 1. New Forest Mouse Species discovered in Sulawesi, Highlighting Indonesian Biodiversity
- 2. Discovery on Mount Tompotika
- 3. Characteristics of *Crunomys owner*
- 4. Taxonomic Revisions in Small Mammal Studies
- 5. Sulawesi: A Hotspot for New Species
- 6. Conservation Implications and Future Research
- 7. The Importance of Biodiversity Hotspots
- 8. Frequently Asked Questions About the New Mouse Species
- 9. What specific genetic markers were used to differentiate the new mouse species from existing Sulawesi rodents?
- 10. New Species of Forest Mice Discovered in Sulawesi by Brin: Insights into Biodiversity in Indonesia’s Unique ecosystems
- 11. The discovery and it’s Significance
- 12. Sulawesi’s Biodiversity Hotspot: A Unique Ecosystem
- 13. Characteristics of the New Mouse Species
- 14. The Role of Brin in Biodiversity research
- 15. Conservation Implications and Threats to sulawesi’s Biodiversity
- 16. future Research Directions
Jakarta – A newly identified species of forest mouse, scientifically named Crunomys owner, has been discovered in the remote mountainous region of Central Sulawesi, Indonesia. The finding, announced on Wednesday by a collaborative research team from the National Research and Innovation Agency (BRIN) and international partners, underscores the island’s exceptional biodiversity and ongoing importance for scientific exploration.
Discovery on Mount Tompotika
The new species was located on Mount tompotika, an area known for its unique ecosystem and relatively undisturbed natural habitats. This discovery forms part of an extensive research initiative examining the systematic arrangement and geographic distribution of mammals across Southeast Asia.Researchers emphasize that indonesia, and Sulawesi in particular, continues to yield new species as exploration efforts intensify.
“This finding significantly expands the documented number of mammals unique to sulawesi,” stated Anang Setiawan Achmadi, a Researcher at BRIN’s Biosystematics and Evolution Research Center. “Continued field studies are consistently revealing new endemic species on the island.”
Characteristics of *Crunomys owner*
The *Crunomys owner* mouse is characterized by its medium size, a tail notably shorter than its body, and the dense fur typical of the Crunomys genus. These creatures inhabit dense, natural mountain forests, specifically those areas less affected by human progress. The conditions provide a natural habitat where they can thrive.
Taxonomic Revisions in Small Mammal Studies
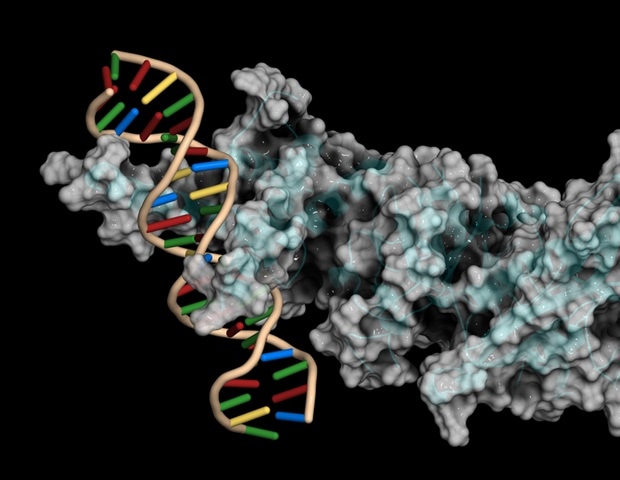
This research also prompted a ample revision in the taxonomy of small mammals. Previously categorized within the Maxomys genus (commonly known as spiny rats), all members have now been reclassified under the Crunomys genus. This reclassification is based on the detailed analysis of high-resolution genomic data.
“Analysis involving thousands of DNA markers, including advanced genomic data, demonstrates that Maxomys does not constitute a cohesive, unified group when considered separately from Crunomys,” explained Achmadi. “The updated classification more accurately reflects the evolutionary relationships among these species.”
Sulawesi: A Hotspot for New Species
Since 2012, over 20 new mammal species have been identified on Sulawesi, highlighting the island’s exceptional biodiversity. This reinforces Sulawesi’s position within the Wallacea region,a globally notable area recognized for its unique and largely unexplored natural diversity.Wallacea, a transition zone between the Australian and Asian faunal regions, is renowned for its high levels of endemism.
| Feature | Crunomys owner | Typical Crunomys Species |
|---|---|---|
| Body Size | Medium | Variable, generally small to medium |
| Tail Length | Shorter than body | Often longer than body |
| Habitat | Dense mountain forests | Varied, including forests and agricultural areas |
| Fur | Dense | Typically dense |
Did You Know? Sulawesi is home to a remarkable number of endemic species – plants and animals found nowhere else on Earth. This makes the island a crucial location for conservation efforts.
Conservation Implications and Future Research
The discovery of the *Crunomys owner* has possibly significant implications for conservation policy. It underscores the need to protect Sulawesi’s unique forest ecosystems.Further research is planned to investigate the ecological role of this new species within the Sulawesi forest ecosystem. Experts hope this research will provide a strong scientific foundation for establishing effective conservation strategies.
“This data is anticipated to be instrumental in strengthening conservation policies and promoting further research into Indonesia’s rich biological heritage,” added Achmadi.
The findings of this study were published on June 13, 2025, in the International Journal of Mammalogy, under the title “Systematics and historical biogeography of Crunomys and Maxomys (Muridae: Murinae), with the description of a new species from Sulawesi and new genus-level classification.”
The Importance of Biodiversity Hotspots
Indonesia, and specifically regions like Sulawesi, are recognized as biodiversity hotspots.These areas harbor a disproportionately large number of endemic species and are under significant threat from habitat loss and other environmental pressures. Understanding and protecting these hotspots is paramount for global conservation efforts.
Pro Tip: Supporting sustainable tourism and responsible land management practices can help conserve biodiversity hotspots like Sulawesi. Choose eco-kind tour operators and advocate for policies that prioritize conservation.
Frequently Asked Questions About the New Mouse Species
- What is *Crunomys owner*? It is a newly discovered species of forest mouse found on Mount Tompotika in Sulawesi, Indonesia.
- why is this discovery critically important? It highlights Sulawesi’s incredible biodiversity and the need for increased conservation efforts.
- What does the name *Crunomys owner* refer to? The name honors the location of its discovery, Mount Tompotika.
- What kind of habitat does this mouse live in? *Crunomys owner* inhabits dense, natural mountain forests.
- How has the classification of related species changed? The Maxomys genus has been reclassified under the Crunomys genus based on genomic analysis.
- how many new mammal species have been discovered on Sulawesi as 2012? More than 20 new mammal species have been found on the island since 2012.
- Where can I find more facts on this research? The findings were published in the International Journal of Mammalogy on June 13, 2025.
what are your thoughts on this incredible discovery? Do you think more resources should be allocated to biodiversity research in Southeast Asia? Share your opinions in the comments below!
What specific genetic markers were used to differentiate the new mouse species from existing Sulawesi rodents?
New Species of Forest Mice Discovered in Sulawesi by Brin: Insights into Biodiversity in Indonesia’s Unique ecosystems
The discovery and it’s Significance
Recent expeditions led by the Russian Academy of Sciences’ P.K. Anokhin Institute of Normal Physiology (Brin) have yielded a remarkable discovery: several new species of forest mice inhabiting the diverse ecosystems of Sulawesi, Indonesia. This finding underscores the island’s status as a biodiversity hotspot and highlights the ongoing need for comprehensive biological surveys in under-explored regions. Sulawesi, known for its unique flora and fauna – including the iconic Sulawesi crested macaque and the maleo bird – continues to reveal its biological secrets. The newly identified muridae species contribute significantly to our understanding of rodent evolution and the complex ecological relationships within Sulawesi’s rainforests.
Sulawesi’s Biodiversity Hotspot: A Unique Ecosystem
Sulawesi’s geographical history has played a crucial role in shaping its exceptional biodiversity. Separated from other major landmasses for millions of years, the island has fostered the evolution of endemic species – those found nowhere else on Earth.
Here’s what makes Sulawesi’s ecosystem so special:
Geological History: Its complex geological formation, resulting from the collision of several tectonic plates, has created a varied landscape of mountains, valleys, and coastal regions.
Isolation: Long-term isolation has allowed unique evolutionary pathways, leading to high levels of endemism.
Rainforests: The island is covered in extensive rainforests, providing habitat for a vast array of species.
Coral Reefs: Surrounding Sulawesi are vibrant coral reefs, contributing to marine biodiversity (as highlighted by Indonesia Travel).
Montane forests: Higher elevations support montane forests with distinct flora and fauna.
This unique combination of factors makes Sulawesi a critical area for conservation efforts. The discovery of new mouse species reinforces the importance of protecting these fragile ecosystems.
Characteristics of the New Mouse Species
While detailed scientific descriptions are still being published, preliminary findings reveal distinct characteristics among the newly discovered mice. These differences extend beyond mere physical appearance and include genetic variations and behavioral patterns.
Morphological Differences: Variations in size, fur color, tail length, and skull morphology distinguish the new species from previously known Sulawesi rodents.
Genetic Analysis: DNA sequencing confirms the genetic distinctiveness of these mice, establishing them as separate species.
Habitat Preference: Each new species appears to occupy a specific ecological niche within the Sulawesi rainforest, demonstrating habitat specialization. Some are found in primary forests,while others inhabit secondary growth or montane regions.
Dietary Habits: Analysis of stomach contents and fecal matter suggests varied diets, ranging from seeds and fruits to insects and invertebrates.
Behavioral Observations: Preliminary observations indicate differences in social behavior, nesting habits, and activity patterns.
The Role of Brin in Biodiversity research
The P.K. Anokhin Institute of Normal Physiology (brin) has a long history of conducting biological research in remote and challenging environments. Their expeditions to Sulawesi are part of a broader effort to document and understand the biodiversity of Indonesia and other Southeast Asian nations.
Brin’s approach typically involves:
- Field Expeditions: Deploying teams of scientists to conduct extensive surveys of flora and fauna.
- Specimen Collection: carefully collecting and preserving specimens for detailed analysis.
- Genetic Sequencing: Utilizing advanced genetic techniques to identify and classify species.
- Ecological Studies: Investigating the ecological roles and interactions of species within their habitats.
- Collaboration: Partnering with local researchers and conservation organizations.
Conservation Implications and Threats to sulawesi’s Biodiversity
The discovery of these new mouse species underscores the urgent need for conservation efforts in sulawesi.The island faces numerous threats to its biodiversity, including:
Deforestation: Logging, agricultural expansion, and mining activities are leading to widespread deforestation, destroying habitats and fragmenting populations.
Hunting: Illegal hunting for bushmeat and customary medicine poses a threat to many species.
Climate Change: Changing climate patterns are altering habitats and disrupting ecological processes.
Habitat Loss: Conversion of forests into agricultural land and settlements.
Illegal Wildlife Trade: Demand for exotic pets and wildlife products fuels illegal trade.
Protecting Sulawesi’s biodiversity requires a multi-faceted approach:
Establishing Protected Areas: Expanding and strengthening the network of national parks and wildlife reserves.
lasting Land Management: Promoting sustainable forestry and agricultural practices.
Community-Based conservation: Engaging local communities in conservation efforts.
Combating Illegal Wildlife Trade: Enforcing laws and regulations to prevent poaching and trafficking.
Raising Awareness: Educating the public about the importance of biodiversity conservation.
future Research Directions
Further research is crucial to fully understand the diversity and ecological roles of Sulawesi’s rodent