“`html
Table of Contents
- 1. Hidden Hypertension: The Growing concern of Normal Readings, Elevated Risk
- 2. The Paradox of Masked Hypertension
- 3. Why Accurate Monitoring Matters
- 4. How might autonomic nervous system dysfunction, commonly observed in type 2 diabetes, contribute to the development of masked hypertension specifically?
- 5. Unveiling Masked Hypertension: Prevalence and Influencing Factors in Type 2 Diabetes Patients
- 6. What is Masked Hypertension?
- 7. Prevalence of Masked Hypertension in Type 2 Diabetes
- 8. Why is Masked Hypertension Hazardous in Diabetics?
- 9. Influencing Factors: What Causes Masked Hypertension?
- 10. Diagnostic Methods: Identifying Masked Hypertension
- 11. Benefits of Early Detection and Management
- 12. Practical Tips for Managing Masked Hypertension
Washington D.C. – A notable number of individuals may be living with undetected High Blood Pressure due to a phenomenon known as masked hypertension,where blood pressure appears normal during doctor’s visits but is consistently high in everyday life. This emerging health concern is prompting renewed attention to more comprehensive blood pressure monitoring practices.
The Paradox of Masked Hypertension
Masked hypertension presents a unique diagnostic challenge. Conventional blood pressure measurements taken in a clinical setting can be artificially lowered due to the “white coat effect,” anxiety associated with medical environments. Consequently,individuals with truly elevated blood pressure outside of the doctor’s office might potentially be missed. The prevalence of this condition is substantial, and estimates suggest it affects a considerable portion of the population, especially those with Type 2 Diabetes.
Recent studies indicate that nocturnal hypertension – High Blood Pressure that is particularly elevated during sleep – is a critical component often missed by standard daytime measurements. This nighttime elevation carries a significantly higher risk of cardiovascular events. According to new data from the american Heart Association, individuals with untreated nocturnal hypertension face a 68% increased risk of stroke and a 42% higher risk of heart attack, compared to those with well-controlled blood pressure throughout the day.
Why Accurate Monitoring Matters
The implications of undiagnosed masked hypertension are far-reaching. untreated High Blood Pressure significantly increases the risk of heart disease, stroke, kidney failure, and other serious health complications. Furthermore,
How might autonomic nervous system dysfunction, commonly observed in type 2 diabetes, contribute to the development of masked hypertension specifically?
Unveiling Masked Hypertension: Prevalence and Influencing Factors in Type 2 Diabetes Patients
What is Masked Hypertension?
Masked hypertension (MHT) refers to normal blood pressure readings in a clinical setting (like a doctor’s office) but elevated blood pressure readings when measured outside of it – typically at home or thru ambulatory blood pressure monitoring (ABPM). This discrepancy poses a meaningful challenge in diagnosing and managing cardiovascular risk, especially in individuals with type 2 diabetes. It’s often called “white coat normotension” in reverse. Understanding masked hypertension in diabetes is crucial because it’s frequently overlooked, yet carries substantial health risks.
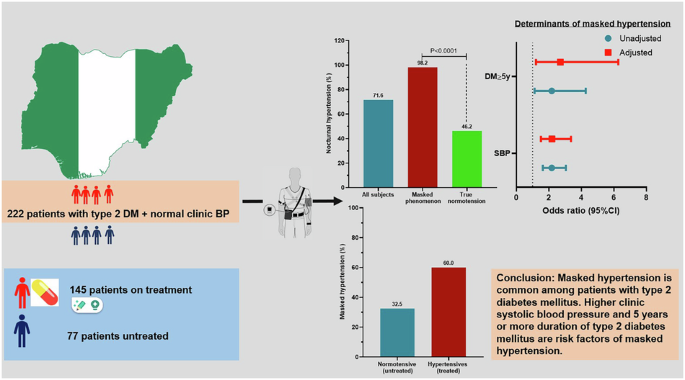
Prevalence of Masked Hypertension in Type 2 Diabetes
The prevalence of MHT is notably higher in individuals with type 2 diabetes compared to the general population. Estimates vary, but studies suggest:
* Overall Prevalence: Approximately 10-30% of individuals with type 2 diabetes exhibit masked hypertension.
* Compared to General Population: This is substantially higher than the 5-10% prevalence seen in those without diabetes.
* Age-Related Increase: Prevalence tends to increase with age, even within the diabetic population.
* Racial and Ethnic Disparities: Some studies indicate higher rates of MHT in certain racial and ethnic groups, highlighting the need for tailored screening approaches.
This increased prevalence underscores the importance of routine blood pressure monitoring beyond the traditional clinical visit.
Why is Masked Hypertension Hazardous in Diabetics?
Diabetics are already at an elevated risk for cardiovascular disease. Masked hypertension exacerbates this risk because:
* Undetected hypertension: Without proper diagnosis, blood pressure remains uncontrolled, leading to progressive organ damage.
* Increased Cardiovascular Events: MHT is associated with a higher incidence of stroke,heart attack,heart failure,and kidney disease.
* Microvascular Complications: Uncontrolled hypertension accelerates diabetic retinopathy and nephropathy.
* Silent Progression: The lack of noticeable symptoms frequently enough allows MHT to progress silently, delaying necessary interventions. Hypertension management is therefore critical.
Influencing Factors: What Causes Masked Hypertension?
Several factors contribute to the development of masked hypertension,particularly in those with type 2 diabetes:
* Autonomic Nervous System Dysfunction: Diabetes can damage the nerves controlling blood pressure regulation,leading to exaggerated responses to stress outside the clinical setting.
* Arterial Stiffness: Increased arterial stiffness, common in diabetes, can cause falsely low readings in the doctor’s office due to the compression of arteries during measurement.
* White Coat Effect (Reverse): While less common, some individuals experience anxiety outside the clinical setting, leading to elevated readings during home or ambulatory monitoring.
* Obesity & Lifestyle factors: Obesity, a sedentary lifestyle, high sodium intake, and excessive alcohol consumption all contribute to hypertension, including masked forms.
* Medication Interference: Certain medications, even over-the-counter drugs, can influence blood pressure readings.
* Glycemic Control: Poorly controlled blood sugar levels can contribute to vascular dysfunction and increased blood pressure variability.
Diagnostic Methods: Identifying Masked Hypertension
Accurate diagnosis is paramount. Relying solely on in-office measurements is insufficient. Key diagnostic tools include:
- Ambulatory Blood pressure Monitoring (ABPM): This is the gold standard. A device worn for 24 hours continuously measures blood pressure at regular intervals, providing a comprehensive picture of blood pressure fluctuations.
- Home Blood Pressure Monitoring (HBPM): Patients measure their blood pressure at home, multiple times a day, over a period of several days. Proper technique is crucial for accurate results. Self-monitoring of blood pressure empowers patients.
- Repeated Office Measurements: while not definitive, consistently normal office readings coupled with risk factors should prompt further investigation with ABPM or HBPM.
Benefits of Early Detection and Management
Early identification and effective management of masked hypertension offer significant benefits:
* Reduced Cardiovascular Risk: Lowering blood pressure reduces the risk of heart attack, stroke, and other cardiovascular events.
* Slowed Progression of Diabetic complications: Controlling hypertension protects the kidneys,eyes,and nerves from further damage.
* Improved Quality of Life: Effective blood pressure management can improve overall well-being and reduce symptoms associated with hypertension.
* Reduced Healthcare Costs: Preventing complications translates to lower healthcare expenses in the long run.
Practical Tips for Managing Masked Hypertension
* Lifestyle Modifications:
* Adopt a heart-healthy diet (DASH diet).
* Engage in regular physical activity (at least 150 minutes of moderate-intensity exercise per week).
* Maintain a healthy weight.
* Limit sodium intake.
* Reduce alcohol consumption.
* Manage stress through techniques like yoga or meditation.
* Medication Adherence: If prescribed, take