The Synaptic Spread of PSP: How New Tau Research Could Rewrite the Future of Dementia Treatment
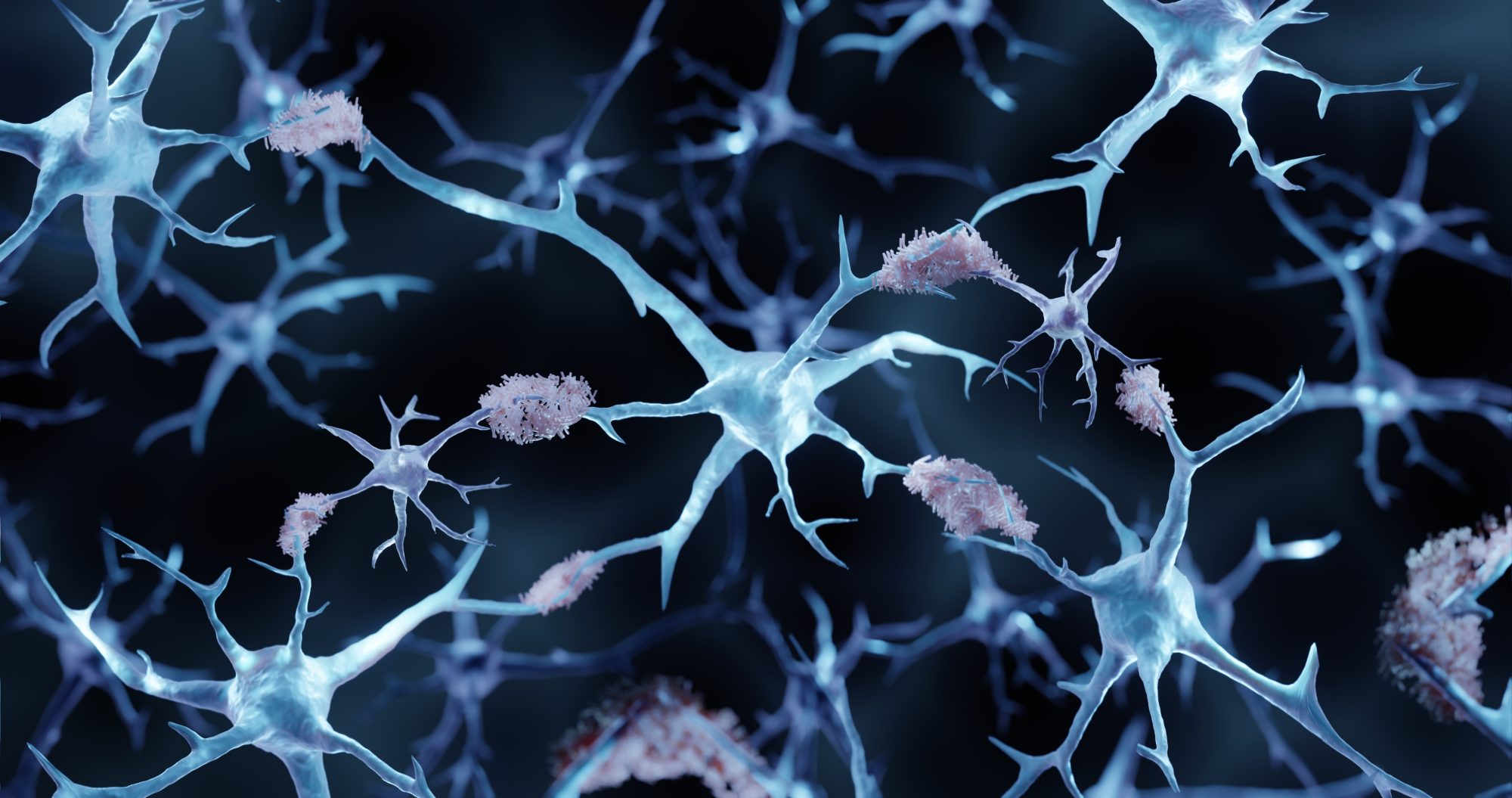
Imagine a scenario where a single, microscopic misstep within the brain’s communication network triggers a cascade of devastating neurological decline. This isn’t science fiction; it’s the reality for individuals living with Progressive Supranuclear Palsy (PSP), a rare but relentlessly progressive neurodegenerative disease. Now, groundbreaking research is revealing precisely how this misstep occurs – the spread of toxic tau proteins through synapses – and, crucially, pinpointing new targets for therapies that could finally halt or slow its progression.
Unraveling the Mystery of Tau’s Journey
PSP affects movement, thinking, and behavior, rapidly stripping individuals of their independence within just a few years of symptom onset. Currently, there are no disease-modifying treatments available. The core problem lies in the accumulation of abnormal tau proteins within neurons. But until recently, the mechanism of spread remained elusive. Scientists knew synapses – the vital connections between neurons – were dying in affected brain regions, but didn’t know if tau directly caused this damage or how it moved between cells.
Recent research from the UK Dementia Research Institute has changed that. Researchers, led by Dr. Robert McGeachan and Dr. Claire Durrant, have demonstrated that tau doesn’t just accumulate within neurons; it actively travels between them, jumping across synapses. This “jumping” occurs via small clumps of tau, moving from the presynapse (the sending side) to the postsynapse (the receiving side). This discovery, published in leading neurological journals, is a pivotal step towards understanding and ultimately combating PSP.
Living Brain Tissue Reveals the Spread in Action
The team’s innovative approach involved using living human brain slices treated with tau protein derived from post-mortem PSP brain tissue. This allowed them to observe the process in a more realistic environment than previously possible. The results were striking: post-synapses readily absorbed the toxic PSP tau. Even more telling, this tau uptake triggered astrocytes – support cells in the brain – to consume the synapses, confirming the toxicity of synaptic tau and the devastating impact of this spread.
Targeting tau in synapses may be the key to slowing disease progression in PSP,” explains Professor Tara Spires-Jones, highlighting the potential for a new generation of therapies.
The Role of Clusterin: A Link to Alzheimer’s?
The research also uncovered a surprising connection to Alzheimer’s disease. The protein clusterin, previously implicated in Alzheimer’s pathology, was found in the same synapses as toxic tau in PSP brain samples. Imaging studies revealed that clusterin and tau are close enough to interact within post-synapses, suggesting clusterin may play a role in either the spread or the toxicity of tau in PSP. This finding opens up intriguing possibilities for repurposing existing Alzheimer’s research and therapies.
Did you know? Clusterin’s presence in both PSP and Alzheimer’s suggests a common underlying mechanism of tau-mediated neurodegeneration, potentially paving the way for broader therapeutic strategies.
Future Trends: From Diagnostics to Targeted Therapies
This breakthrough isn’t just about understanding PSP; it’s a paradigm shift in how we approach tau-related neurodegenerative diseases. Here’s what we can expect to see in the coming years:
- Enhanced Diagnostics: The ability to detect synaptic tau spread could lead to earlier and more accurate diagnoses of PSP and potentially other tauopathies. New biomarkers, detectable through cerebrospinal fluid analysis or advanced brain imaging techniques, are actively being developed.
- Synaptic Protection Strategies: Research will increasingly focus on protecting synapses from tau toxicity. This could involve developing drugs that prevent tau from entering synapses, stabilize synaptic connections, or enhance the ability of synapses to clear tau.
- Clusterin Modulation: Given its potential role in tau pathology, clusterin is emerging as a promising therapeutic target. Strategies to modulate clusterin activity – either increasing or decreasing its levels – could offer a novel approach to slowing disease progression.
- Personalized Medicine: As we learn more about the genetic and environmental factors that influence PSP, personalized treatment approaches will become increasingly important. Tailoring therapies to individual patient profiles could maximize efficacy and minimize side effects.
Expert Insight: “The use of human tissue, as demonstrated in this study, is crucial for ensuring that preclinical findings translate effectively to patients,” says Dr. Claire Durrant. “As dementia research advances, this approach will become increasingly vital.”
The Rise of ‘Synaptic-Focused’ Drug Development
For decades, much of the focus in neurodegenerative disease research has been on the accumulation of amyloid plaques or tau tangles within neurons. However, this new research underscores the critical importance of synapses – the very foundation of brain function. We’re likely to see a surge in drug development efforts specifically targeting synaptic health and preventing tau-mediated synaptic damage. This represents a fundamental shift in therapeutic strategy.
Pro Tip: Stay informed about clinical trials related to PSP and other tauopathies. Participating in research is a valuable way to contribute to the advancement of knowledge and potentially access cutting-edge treatments.
Implications Beyond PSP: A Broader Impact on Dementia Research
While this research specifically focuses on PSP, the mechanisms of tau spread identified have implications for other neurodegenerative diseases, including Alzheimer’s disease, chronic traumatic encephalopathy (CTE), and frontotemporal dementia. Tau pathology is a common feature of these conditions, and understanding how tau spreads between neurons is crucial for developing effective therapies for all of them.
Key Takeaway: The discovery of synaptic tau spread represents a major breakthrough in our understanding of PSP and offers a new avenue for therapeutic intervention. This research has far-reaching implications for the broader field of dementia research.
Frequently Asked Questions
Q: What are the current treatment options for PSP?
A: Currently, there are no treatments available that can slow or stop the progression of PSP. Treatment focuses on managing symptoms and improving quality of life.
Q: How is PSP diagnosed?
A: PSP diagnosis can be challenging, as symptoms can overlap with other neurological conditions. Diagnosis typically involves a neurological examination, brain imaging (MRI), and sometimes a dopamine transporter scan.
Q: Is PSP genetic?
A: While most cases of PSP are sporadic (occurring randomly), a small percentage are linked to genetic mutations. Research is ongoing to identify genes that may increase the risk of developing PSP.
Q: What can I do to support PSP research?
A: You can support PSP research by donating to organizations dedicated to funding research, participating in clinical trials, or raising awareness about the disease.
What are your thoughts on the future of PSP treatment? Share your perspective in the comments below!