The Dawn of Digital Dementia Screening: How AI and Blood Tests Are Revolutionizing Alzheimer’s Diagnosis
Imagine a future where a 15-minute check-up at your family doctor could offer a surprisingly accurate glimpse into your risk of developing Alzheimer’s disease. That future is closer than you think. Researchers at Lund University in Sweden have developed BioCog, a self-administered digital cognitive test, poised to dramatically reshape early Alzheimer’s detection and, crucially, determine who will benefit from emerging disease-modifying treatments.
The Challenge of Early Detection & The Promise of Precision
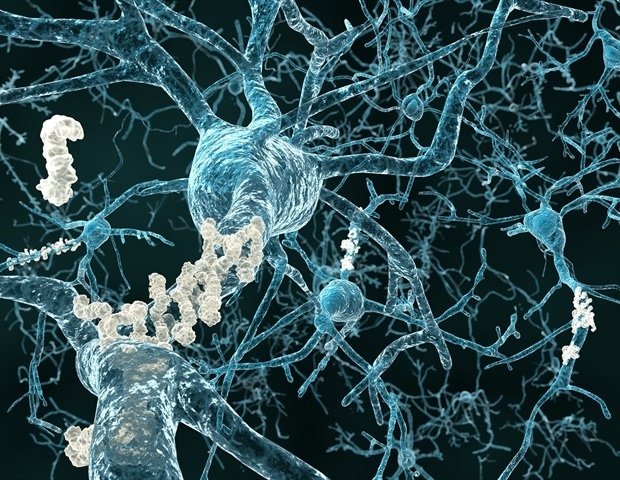
For decades, diagnosing Alzheimer’s has been a complex, often delayed process. Traditional pen-and-paper cognitive assessments are subjective and lack the granularity needed for early identification. The stakes are higher than ever. With new drugs like lecanemab and donanemab showing promise in slowing disease progression, identifying patients before significant brain damage occurs is paramount. However, these treatments aren’t universally effective, making accurate diagnosis even more critical. According to the Alzheimer’s Association, over 6.7 million Americans are living with Alzheimer’s disease in 2023, and that number is projected to rise sharply in the coming decades.
“Primary care does not have the resources, time or specialist knowledge to investigate possible Alzheimer’s disease in the same way as specialised memory clinics,” explains Professor Oskar Hansson of Lund University. “And this is where a digital cognitive test can make the biggest difference.” BioCog aims to bridge that gap, providing a resource-efficient first step in the diagnostic pathway.
How BioCog Works: Beyond Pen and Paper
BioCog isn’t just a digital version of existing tests. It leverages the power of technology to capture a more nuanced picture of cognitive function. Patients complete the test independently on a tablet, assessing:
- Memory: Memorizing ten words.
- Cognitive Processing Speed & Attention: How quickly information is processed.
- Orientation: Recall of current date and year.
- Delayed Recall: Recalling previously memorized information.
- Recognition: Identifying memorized words from a larger list.
Unlike traditional methods, BioCog tracks how a patient arrives at an answer – the time taken to search for words, the speed of screen taps – providing data points previously inaccessible. This detailed analysis, combined with a subsequent blood test measuring phosphorylated tau levels (a key biomarker for Alzheimer’s pathology), significantly increases diagnostic accuracy.
The Blood Test Breakthrough: From Specialist Clinics to Primary Care
Currently, blood tests for Alzheimer’s biomarkers are largely confined to specialized memory clinics. However, the ultimate goal is to make these tests more widely available. BioCog acts as a crucial filter, identifying patients who would most benefit from this more advanced testing, preventing unnecessary strain on healthcare resources. This tiered approach – digital screening followed by targeted biomarker analysis – represents a significant shift in Alzheimer’s care.
The Future of Cognitive Assessment: AI, Wearables, and Personalized Medicine
BioCog is just the beginning. The convergence of digital cognitive testing, advanced biomarkers, and artificial intelligence is poised to revolutionize how we understand and manage cognitive decline. Here’s what we can expect to see in the coming years:
AI-Powered Predictive Models
The data generated by tests like BioCog will fuel the development of sophisticated AI algorithms capable of predicting an individual’s risk of developing Alzheimer’s years before symptoms manifest. These predictive models could identify individuals who would benefit from early interventions, such as lifestyle modifications or preventative therapies.
Wearable Technology & Continuous Monitoring
Imagine a smartwatch that continuously monitors subtle changes in cognitive function – sleep patterns, speech patterns, reaction times – providing a constant stream of data to healthcare providers. Wearable sensors, coupled with AI analysis, could offer an unprecedented level of personalized cognitive monitoring. See our guide on the latest advancements in wearable health technology for more information.
Personalized Treatment Strategies
As we gain a deeper understanding of the underlying causes of Alzheimer’s disease, treatment strategies will become increasingly personalized. Genetic testing, biomarker analysis, and cognitive assessments will be used to tailor therapies to the specific needs of each patient, maximizing their chances of success.
The Ethical Considerations
The rise of predictive diagnostics also raises important ethical questions. How do we ensure that individuals are adequately informed about their risk of developing Alzheimer’s? How do we protect against genetic discrimination? These are complex issues that will require careful consideration as these technologies become more widespread.
Frequently Asked Questions
What is the benefit of a digital cognitive test over traditional methods?
Digital tests like BioCog offer greater precision and detail, capturing subtle cognitive changes that may be missed by traditional pen-and-paper assessments. They also provide objective data, reducing the potential for subjective bias.
Will this test be available to everyone?
The initial rollout will likely focus on integrating BioCog into primary care settings. Wider availability will depend on factors such as cost, accessibility, and healthcare infrastructure.
What if the test indicates a potential risk of Alzheimer’s?
A positive result on BioCog doesn’t necessarily mean you have Alzheimer’s. It indicates a need for further evaluation, including a blood test to assess Alzheimer’s biomarkers. A healthcare professional will interpret the results and discuss appropriate next steps.
How accurate is BioCog?
Studies have shown that BioCog, when combined with blood biomarker analysis, significantly improves the accuracy of Alzheimer’s diagnosis. The test has been specifically validated in a primary care population, making it a reliable tool for initial screening.
The development of BioCog marks a pivotal moment in the fight against Alzheimer’s disease. By empowering primary care physicians with accessible, accurate diagnostic tools, we are one step closer to a future where early detection and personalized treatment can transform the lives of millions affected by this devastating condition. What are your thoughts on the role of technology in revolutionizing healthcare? Share your perspective in the comments below!