Epac1 Inhibition: A New Frontier in Fighting Idiopathic Pulmonary Fibrosis
Imagine a future where the relentless scarring of lungs, the hallmark of idiopathic pulmonary fibrosis (IPF), could be significantly slowed, offering patients precious years of improved quality of life. Researchers at the Icahn School of Medicine at Mount Sinai have pinpointed a previously overlooked protein, Epac1, as a key driver of this devastating disease, and crucially, demonstrated that blocking it can halt its progression. This discovery isn’t just another incremental step; it’s a potential paradigm shift in how we approach IPF treatment.
The Silent Scourge of IPF and the Search for New Targets
Idiopathic pulmonary fibrosis affects an estimated 140,000 to 200,000 Americans, with a median survival rate of just 3-5 years after diagnosis. The disease causes progressive scarring of the lungs, making it increasingly difficult to breathe and ultimately leading to respiratory failure. Current treatments offer limited benefits, primarily focusing on slowing disease progression rather than reversing the damage. This urgent need for more effective therapies fueled the Mount Sinai team’s investigation into the role of Epac1.
Unveiling Epac1’s Harmful Role in Lung Fibrosis
“We were motivated by the urgent need for new therapies,” explains Dr. Lahouaria Hadri, co-senior corresponding author of the study. “We focused on Epac1 because we suspected this little-known protein might be doing more harm than previously thought in fibrotic lungs—and that turned out to be the case.” The research, published in the European Respiratory Journal, revealed that Epac1 is significantly overactive in the lungs of IPF patients. When the researchers genetically removed Epac1 in mice, or treated lung tissue with the drug AM-001, designed to inhibit the protein, they observed a marked reduction in lung scarring and fibrosis.
Neddylation: A New Piece of the IPF Puzzle
The study’s significance extends beyond simply identifying Epac1 as a target. Researchers also discovered a link between Epac1 activity and a biological process called “neddylation,” which regulates protein function. This connection provides a deeper understanding of the molecular mechanisms driving IPF. Understanding how Epac1 interacts with neddylation could unlock even more targeted therapeutic strategies.
The Promise of AM-001 and Future Drug Development
The small-molecule drug AM-001, used in the study to inhibit Epac1, shows considerable promise. While still in the preclinical stage, its effectiveness across cell cultures, mouse models, and human lung tissue is highly encouraging. However, Dr. Hadri cautions that extensive testing is still required. “This is early-stage, preclinical research,” she states. “Much more work, including testing in larger animal models and eventual clinical trials, is needed before Epac1 inhibitors like AM-001 can be developed into a therapy for patients.”
Beyond AM-001: The Future of Targeted IPF Therapies
The identification of Epac1 as a key driver of IPF opens up several exciting avenues for future research and treatment development. Here are some potential trends to watch:
- Personalized Medicine Approaches: Genetic testing could identify individuals at higher risk of developing IPF due to variations in Epac1 or related genes, allowing for early intervention and preventative strategies.
- Combination Therapies: Combining Epac1 inhibitors with existing IPF treatments could offer synergistic benefits, maximizing therapeutic efficacy.
- Biomarker Development: Identifying biomarkers that indicate Epac1 activity levels could help monitor disease progression and treatment response.
- Expanding the Scope: Researchers are already exploring whether Epac1 plays a role in other fibrotic diseases, such as systemic sclerosis and liver fibrosis, potentially broadening the impact of this discovery.
The Role of AI and Machine Learning in Accelerating IPF Research
The complexity of IPF and the vast amount of data generated by research efforts are creating opportunities for artificial intelligence (AI) and machine learning (ML). AI algorithms can analyze complex datasets to identify patterns and predict treatment responses, accelerating the drug discovery process. For example, ML models could be used to screen potential drug candidates for their ability to inhibit Epac1 or to predict which patients are most likely to benefit from Epac1-targeted therapies. Mount Sinai is already at the forefront of using AI in cancer research, and similar approaches could be applied to IPF.
Expert Insight:
“The discovery of Epac1’s role in IPF is a game-changer. It provides a new, highly specific target for drug development, and the link to neddylation offers a deeper understanding of the disease’s underlying mechanisms. While challenges remain, this research represents a significant step forward in our fight against this devastating condition.” – Dr. Emily Carter, Pulmonary Specialist.
Frequently Asked Questions
- What is idiopathic pulmonary fibrosis (IPF)?
- IPF is a chronic and progressive lung disease characterized by scarring of the lungs, making it difficult to breathe. The cause is often unknown (idiopathic).
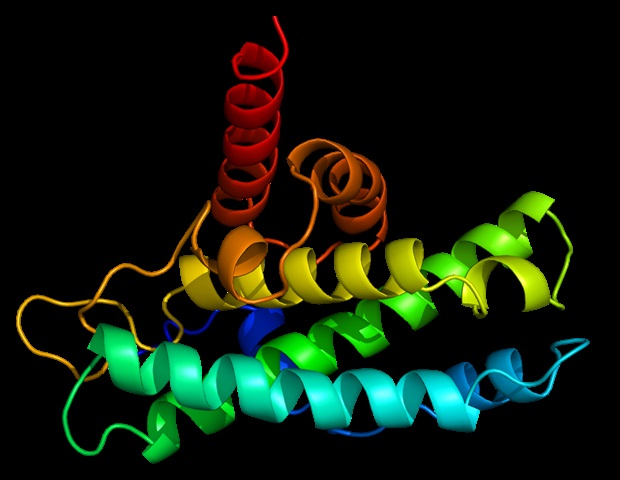
- What is Epac1 and why is it important?
- Epac1 is a protein that researchers have now identified as a key driver of IPF. Blocking Epac1 has been shown to slow the progression of the disease in preclinical studies.
- How far away is a potential treatment based on Epac1 inhibition?
- While promising, research is still in the preclinical stage. Extensive testing, including clinical trials, is needed before Epac1 inhibitors can become available to patients.
- Are there any lifestyle changes I can make to reduce my risk of IPF?
- While there’s no known way to prevent IPF, avoiding smoking and exposure to certain environmental pollutants may reduce your risk. If you experience persistent shortness of breath, consult a doctor.
The research surrounding Epac1 and IPF is a beacon of hope for those affected by this debilitating disease. As research progresses and new therapies are developed, the prospect of a future with improved outcomes for IPF patients becomes increasingly attainable. What are your thoughts on the potential of targeted therapies like Epac1 inhibition? Share your perspective in the comments below!