Recent research has unveiled significant insights into the innate antiviral and immune functions associated with HIV reservoir decay following anti-PD-1 therapy. This innovative study explored the effects of pembrolizumab, an anti-PD-1 monoclonal antibody, on individuals living with HIV and advanced cancer. The findings indicate promising avenues for enhancing immune responses that could contribute to HIV management.
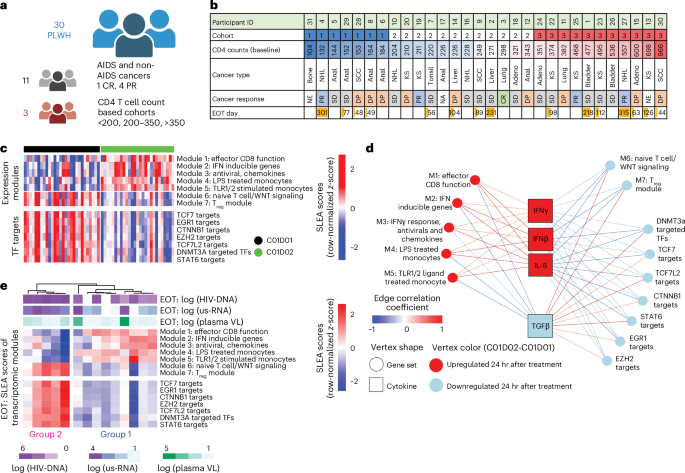
The study involved 30 virally suppressed participants, predominantly male, who were subjected to a regimen of pembrolizumab administered every three weeks for up to two years. Researchers observed notable clinical benefits, including reductions in HIV reservoirs and positive responses to cancer treatments, suggesting a dual efficacy of anti-PD-1 therapy in managing both cancer and HIV, as evidenced by measurable changes in CD4+ T cell counts.
Understanding the Study Design
The research was part of the CITN-12 trial (NCT02595866), a multicenter, open-label, non-randomized phase 1 study that adhered to ethical standards outlined in the Declaration of Helsinki. The study protocol received approval from multiple institutional review boards, ensuring participant safety, and confidentiality. Comprehensive informed consent was obtained prior to enrollment, allowing for a thorough investigation of the immunological effects of the therapy.
Key Findings on Immune Responses
Participants were stratified into three cohorts based on their baseline CD4+ T cell counts: 100−199, 200−350, and over 350 cells per microliter. Throughout the study, blood samples were collected at various time points—before treatment, 24 hours after treatment, one week after treatment, and at the end of the treatment period. This longitudinal sampling enabled researchers to monitor changes in plasma cytokines and viral loads meticulously.
Utilizing advanced techniques such as bulk RNA sequencing and single-cell RNA sequencing, the study revealed substantial transcriptomic shifts among participants. Notably, the analysis highlighted an increase in antiviral signaling pathways, including the activation of genes crucial for restricting HIV replication. The findings correlate with earlier studies indicating that reductions in HIV DNA and transcription levels can occur within the first week of anti-PD-1 therapy.
Implications for HIV Management
The study contributes to the understanding of how immune modulation through anti-PD-1 therapy may enhance innate antiviral responses. The documented reduction in HIV reservoirs and the subsequent immune rebound suggest potential strategies for managing HIV beyond traditional antiretroviral therapies. This dual approach of treating cancer while simultaneously addressing HIV could reshape therapeutic paradigms for patients with coexisting conditions.
Researchers likewise emphasized the importance of cytokine profiling, noting how specific cytokines correlated inversely with inflammatory responses. The plasma cytokine levels, including various interleukins and growth factors, were meticulously quantified, revealing a complex interplay between immune activation and HIV reservoir dynamics.
What Lies Ahead
This groundbreaking research underscores the importance of continued exploration into immune therapies for HIV. As the medical community seeks to improve treatment regimens for patients facing both HIV and cancer, the implications of these findings may pave the way for innovative therapeutic strategies. Future studies will likely focus on larger cohorts and longer-term outcomes to validate these promising results further.
As researchers refine their understanding of immune mechanisms in HIV management, the potential for enhanced therapeutic approaches continues to grow. Engaging discussions around these findings are encouraged, and readers are invited to share their thoughts and insights.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional for questions regarding medical conditions or treatments.