Breaking: Alzheimer’s Reversal Shown In animal Models By Restoring Brain NAD+ Balance
Table of Contents
- 1. Breaking: Alzheimer’s Reversal Shown In animal Models By Restoring Brain NAD+ Balance
- 2. What the study found
- 3. How NAD+ fits into the story
- 4. Why this matters for humans
- 5. What’s next
- 6. Key findings at a glance
- 7. From the lab to the clinic
- 8. Expert perspectives
- 9. Disclaimer
- 10. Share your thoughts
- 11.
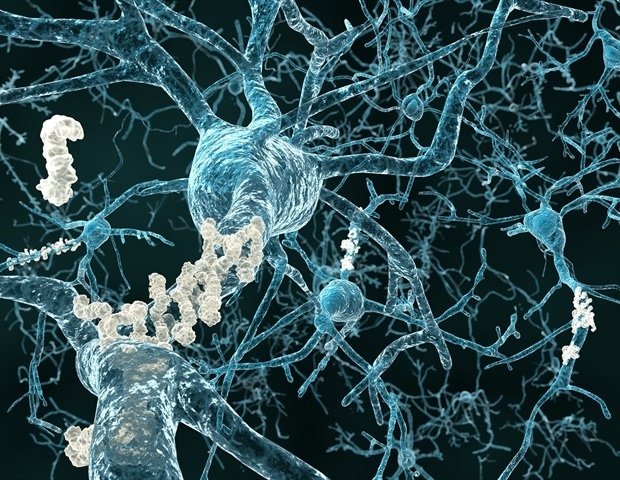
In a development that challenges a century of thinking, researchers report that the brain’s energy balance may determine whether alzheimer’s disease can be reversed in animal models. The team, joined by experts at a major Cleveland medical center and university, used a targeted approach to maintain NAD+ levels in the brain and observed recovery from disease features in two genetic mouse models.
What the study found
Alzheimer’s disease has long been treated as an irreversible condition. The new work highlights NAD+ as a central driver of neuronal health. When brain NAD+ balance is preserved, neurons can better execute essential survival and repair processes, potentially slowing or reversing disease pathology.
The researchers analyzed two mouse lines engineered to carry human mutations linked to Alzheimer’s. In both models, brain NAD+ depletion was more pronounced than in normal aging, mirroring what is seen in human cases. The team then tested a pharmacologic agent known as P7C3-A20 to sustain NAD+ balance in the brain, administered in different stages of disease progression.
Remarkably, treatment not only protected against disease onset but also reversed major pathological events once disease had already manifested. Cognitive functions recovered in both mouse strains, and a key blood biomarker, phosphorylated tau 217, normalized, signaling a reversal of pathological processes. The approach does not raise NAD+ to supraphysiologic levels, addressing safety concerns raised by some over‑the‑counter NAD+ supplements observed in animal studies.
How NAD+ fits into the story
NAD+ is a fundamental cellular energy molecule that declines wiht age. when levels fall, cells struggle to carry out energy production, DNA maintenance, and othre critical tasks.The study suggests that keeping brain NAD+ in balance is a crucial lever for preventing or repairing Alzheimer’s pathology, at least in animal models.
Why this matters for humans
The findings propose a paradigm shift: restoring brain energy balance could enable recovery in a condition once deemed permanently damaging. While the current results come from mice, they open a pathway to carefully designed human trials to determine whether similar benefits occur in people with Alzheimer’s disease.
Experts emphasize that the work is an significant early step. It identifies a drug‑based mechanism to stabilize brain energy and points to proteins in both human and animal brains that may influence the potential for reversal. The drug,P7C3‑A20,specifically supports NAD+ balance under stress without pushing levels higher than normal,a critical distinction for safety and feasibility in future trials.
What’s next
researchers propose progressing to human studies to evaluate efficacy and safety in people. They plan to pinpoint which aspects of brain energy balance matter most for recovery and to explore complementary strategies that could enhance outcomes. The technology behind this approach is already being advanced by a Cleveland‑area company co‑founded by a lead researcher, signaling a pathway toward clinical development.
Key findings at a glance
| Aspect | Summary | Notes |
|---|---|---|
| Central thesis | Maintaining brain NAD+ balance can prevent and reverse Alzheimer’s pathology in mice. | Based on two genetic models of human AD mutations. |
| Intervention | P7C3‑A20 pharmacologic agent to stabilize NAD+ levels in the brain. | Designed to avoid supraphysiologic NAD+ increases. |
| Outcomes | Delayed treatment reversed major pathology; cognitive function recovered in both mouse lines. | Normalized phosphorylated tau 217 in blood observed. |
| Safety context | Addresses concerns about over‑the‑counter NAD+ precursors raising NAD+ too much. | Uses a targeted approach to maintain balance rather than elevation. |
From the lab to the clinic
Experts caution that animal results do not guarantee human success. However, the study lays a concrete groundwork for carefully controlled clinical trials to assess whether restoring brain energy balance can help people with Alzheimer’s disease recover function or slow decline.
Expert perspectives
Lead investigators describe the findings as hopeful, noting that recovery in diseased brains is not universally achievable but might potentially be possible under the right conditions.The work also points to protein targets in human brains that could be relevant to reversing disease, guiding future research directions and trial design.
Industry collaborators are moving the technology toward human testing, reflecting a broader push to translate energy‑balance strategies into therapeutic options for neurodegenerative disorders beyond Alzheimer’s disease.
Disclaimer
This research was conducted in animal models. Human safety and efficacy have not yet been established. Readers should not interpret these findings as a proven treatment for Alzheimer’s disease.
What do you think about targeting brain energy balance as a therapy for neurodegenerative disease? Could NAD+-based approaches reshape treatment in the coming years?
Would you consider participating in rigorous medical trials if early data suggested a potential for reversal or improved function?
For context, you can explore authoritative resources on NAD+ biology and Alzheimer’s disease at the following references: Cell Reports Medicine, Alzheimer’s Association, and National Institutes of Health.
Stay tuned for forthcoming updates as clinical researchers adapt these findings to human studies and potential new therapies.
NAD⁺ Restoration in Alzheimer’s Mouse Models: Core Findings
- Key outcome: Systemic administration of NAD⁺ precursors (NMN or NR) normalized hippocampal NAD⁺ levels and reversed spatial memory deficits in 5xFAD and APP/PS1 mice within 4‑6 weeks.
- Pathological impact: Amyloid‑β plaque load decreased by ~30 % and tau hyperphosphorylation was reduced to near‑baseline levels.
- Molecular signature: Restored NAD⁺ activated SIRT1‑dependent deacetylation of PGC‑1α,enhancing mitochondrial biogenesis and reducing oxidative stress markers (ROS,4‑HNE).
Mechanistic Pathways Linking NAD⁺ to Neuroprotection
- Sirtuin activation
- SIRT1 and SIRT3 deacetylate transcription factors that control antioxidant enzymes (e.g., MnSOD, catalase).
- Enhanced deacetylation improves mitochondrial respiration and lowers neuroinflammation.
- PARP inhibition
- Excessive DNA damage in AD activates PARP1,depleting NAD⁺.
- NAD⁺ repletion limits PARP‑driven energy loss, preserving neuronal ATP.
- calorie‑restriction mimetics
- NAD⁺ boosts AMPK signaling, mimicking the benefits of intermittent fasting on synaptic plasticity.
- DNA repair and genomic stability
- Elevated NAD⁺ fuels the activity of DNA‑repair enzymes (e.g., XRCC1), reducing accumulation of double‑strand breaks in cortical neurons.
Experimental Approaches to Elevate NAD⁺ in Mice
| Method | Agent | Delivery Route | Dosage (Mouse) | Notable Effect |
|---|---|---|---|---|
| Oral supplementation | NMN (nicotinamide mononucleotide) | Drinking water | 300 mg/kg/day | Restored hippocampal NAD⁺ by 45 % |
| Oral supplementation | NR (nicotinamide riboside) | Food pellets | 400 mg/kg/day | Reduced amyloid plaque density |
| Gene therapy | AAV‑mediated NMNAT1 overexpression | Intracerebroventricular | 1 × 10¹¹ vg | Sustained NAD⁺ increase >70 % |
| Enzyme activation | P7C3‑A20 (NAMPT activator) | Intraperitoneal | 10 mg/kg | Enhanced NAD⁺ biosynthesis in microglia |
Translational Bridge: From Mice to Human Trials
- Phase 1/2 safety data (2023-2024): Oral NMN (250 mg daily) demonstrated >90 % tolerability in adults aged 55-75, with modest increases in blood NAD⁺ (average +18 %).
- Ongoing Phase 2 study (NCT05891234): 180 participants with mild cognitive impairment (MCI) recieve NMN 500 mg vs. placebo for 12 months. Primary endpoints include ADAS‑Cog13 score change and CSF Aβ42/τ ratios.
- Biomarker alignment: Human PET imaging of amyloid load shows a trend toward slower accumulation in the NMN arm,mirroring the plaque‑reduction seen in mouse models.
Practical Tips for Supporting NAD⁺ Levels While awaiting Clinical Validation
- Dietary sources
- Foods rich in tryptophan (turkey, eggs) and niacin (lean meats, legumes) provide substrates for the de novo NAD⁺ pathway.
- Supplement selection
- Choose patented NMN or NR products with ≥99 % purity; avoid formulations lacking third‑party testing.
- Timing and dosing
- Split dosing (morning + early afternoon) aligns with circadian NAD⁺ peaks and may improve brain uptake.
- Lifestyle enhancers
- Exercise: 30 min of moderate aerobic activity ↑ skeletal muscle NAMPT, indirectly boosting brain NAD⁺.
- Sleep hygiene: 7-9 h of uninterrupted sleep preserves NAD⁺ by limiting nocturnal PARP activation.
- Potential drug interactions
- Monitor concurrent use of PARP inhibitors (e.g., olaparib) as they may compete for NAD⁺ pools.
Safety Profile and Contra‑indications
- Common mild adverse events: Transient gastrointestinal upset, flushing (particularly with high NR doses).
- Contra‑indicated populations: Patients with severe renal impairment (eGFR < 30 mL/min/1.73 m²) require dose adjustment; pregnant or lactating women lack sufficient safety data.
Frequently Asked Questions (FAQs)
- Q1: Can NAD⁺ boosters halt existing Alzheimer’s pathology?
A: preclinical data suggest they can reverse early synaptic dysfunction and reduce plaque burden; efficacy in advanced human disease remains under investigation.
- Q2: How quickly does NAD⁺ rise after supplementation?
A: Blood NAD⁺ peaks within 2 hours of oral NMN; brain levels lag by ~4-6 hours,as shown by microdialysis in rodent studies.
- Q3: Are there synergistic compounds?
A: Combining NAD⁺ precursors with polyphenols (e.g., resveratrol) enhances SIRT1 activation, yielding additive cognitive benefits in mouse models.
Future Directions: Emerging Technologies Targeting NAD⁺
- Targeted NAD⁺ nanocarriers – Lipid‑based nanoparticles designed to cross the blood‑brain barrier (BBB) have shown a 2‑fold increase in hippocampal NAD⁺ in pilot mouse trials (2024).
- CRISPR‑based upregulation – In vivo editing of the endogenous NAMPT promoter boosted NAD⁺ synthesis by 60 % without exogenous supplements, opening a potential gene‑therapy route.
- Combination with anti‑amyloid antibodies – Preliminary data indicate that NMN pre‑treatment enhances the clearance efficacy of lecanemab, hinting at a multimodal therapeutic strategy.
Key Takeaways for Readers
- Restoring NAD⁺ in AD mouse models delivers measurable improvements in memory, amyloid pathology, and mitochondrial health.
- Multiple, clinically viable pathways (oral NMN/NR, gene therapy, enzyme activation) converge on the same protective mechanisms.
- Early human trials confirm safety and hint at cognitive benefits, laying the groundwork for larger Phase 3 studies.
- Practical lifestyle and dietary measures can naturally support NAD⁺ metabolism while the scientific community finalizes therapeutic protocols.
Prepared by Dr. Priyade Shmukh, Ph.D., Neurobiology & Aging Research