Glaucoma Surgery: Newer Procedures Linked to Lower Risk of Corneal Complications
Table of Contents
- 1. Glaucoma Surgery: Newer Procedures Linked to Lower Risk of Corneal Complications
- 2. The Study Findings
- 3. Comparing Glaucoma Surgical Approaches
- 4. Limitations and Future Directions
- 5. Understanding Glaucoma and Surgical Options
- 6. Frequently Asked questions about Glaucoma surgery
- 7. What are the primary mechanisms by which GDD implantation can lead to corneal edema?
- 8. Corneal Edema Risk Rises with glaucoma Drainage Device Use
- 9. Understanding Glaucoma Drainage Devices (gdds) and Corneal Health
- 10. Why gdds Can Lead to Corneal Edema
- 11. Identifying Corneal Edema: Symptoms and Diagnosis
- 12. management Strategies for Corneal Edema Post-GDD
- 13. Proactive Measures & Prevention
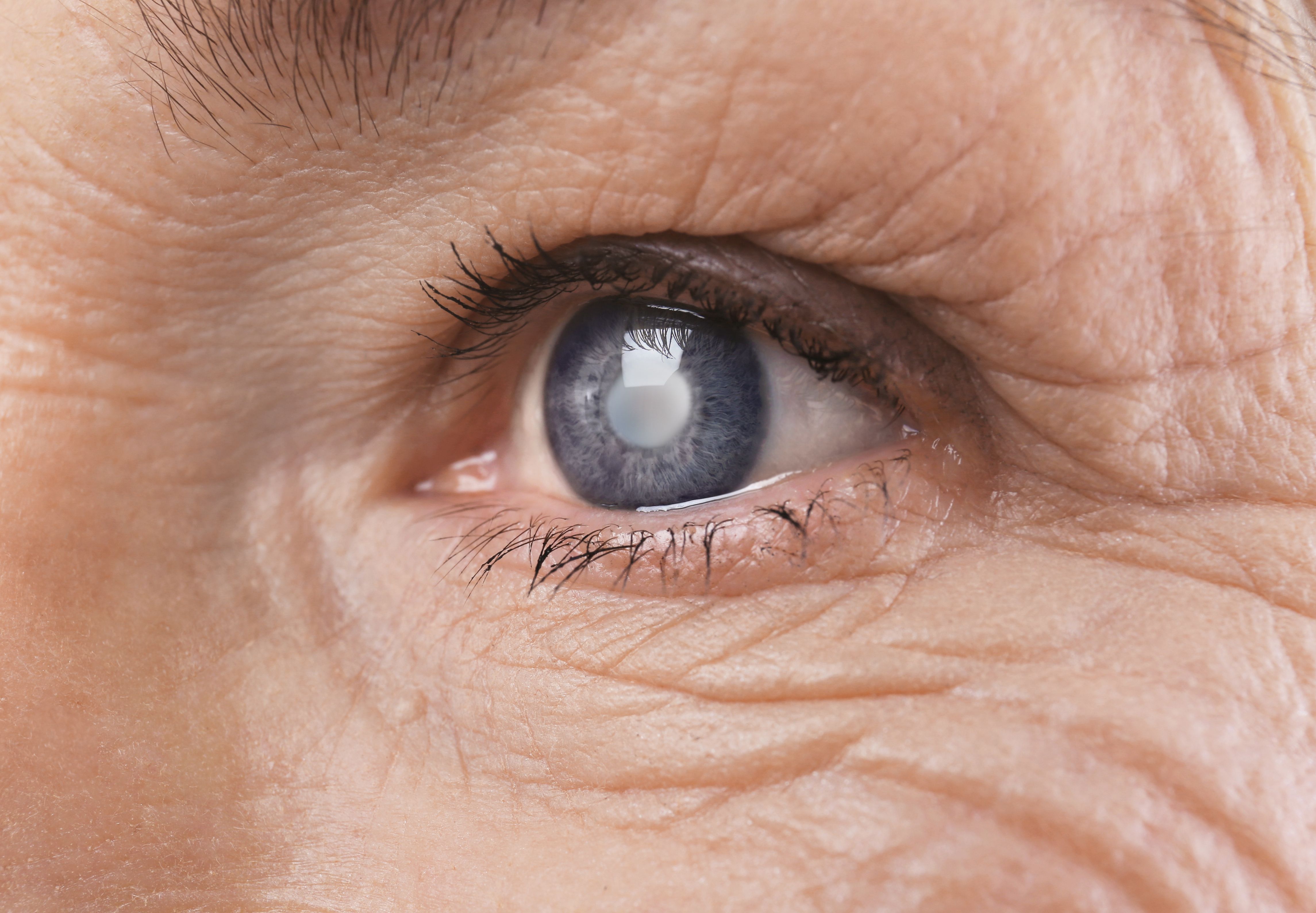
Kingston, Canada – A new study has identified a heightened risk of corneal edema – swelling of the cornea – following glaucoma surgery when glaucoma drainage devices (GDDs) are utilized. The findings, stemming from a retrospective analysis conducted at Kingston health Sciences Center, suggest that minimally invasive glaucoma surgery (MIGS) and Xen stents offer preferable alternatives with markedly reduced complication rates. This is a critical development as glaucoma affects an estimated 79 million people worldwide,with projections indicating 111.8 million will be impacted by 2040.
The Study Findings
Researchers meticulously reviewed data from 333 eyes, representing 245 patients, who underwent glaucoma surgery between January 2005 and August 2024. The average follow-up period was 4.7 years, with a mean patient age of 73.9 years at the time of surgery. The examination focused on comparing the incidence of corneal edema across different surgical techniques: GDDs, trabeculectomy, Xen stents, and MIGS.
The results demonstrated a considerable difference in corneal edema rates. Patients receiving GDDs experienced an edema incidence of 27.7%, significantly higher than the 13.5% observed with trabeculectomy. Notably, Xen stents exhibited a very low rate of 0.98%, and MIGS showed an even lower rate of 1.1%. statistical analysis confirmed that GDDs increased the risk of corneal edema by more than threefold compared to trabeculectomy.
Comparing Glaucoma Surgical Approaches
The primary goal of all glaucoma surgeries is to reduce intraocular pressure (IOP). However, the methods to achieve this reduction carry varying risks. The following table summarizes the key findings regarding corneal edema risk:
| Surgery Type | Corneal Edema Incidence (%) |
|---|---|
| Glaucoma Drainage Devices (GDDs) | 27.7 |
| Trabeculectomy | 13.5 |
| Xen stents | 0.98 |
| MIGS | 1.1 |
Did You Know? Corneal edema can significantly impair vision and may require additional treatment, including corneal transplants, in severe cases.
Limitations and Future Directions
The study acknowledges certain limitations, including its retrospective design and the possibility of incomplete documentation, which could have influenced the accuracy of edema classifications.Additionally, patients undergoing MIGS and Xen procedures had comparatively shorter follow-up periods. The research was also conducted at a single center, perhaps limiting the generalizability of the findings.
Despite these caveats,the authors emphasize the importance of prolonged monitoring for glaucoma patients,especially those undergoing multiple surgeries or receiving GDDs,due to their elevated risk of complications. Further research with larger, multi-center cohorts is needed to confirm these findings and refine surgical protocols.
Pro Tip: If you are diagnosed with glaucoma, open communication with your ophthalmologist about the various treatment options and their potential risks and benefits is vital.
Understanding Glaucoma and Surgical Options
glaucoma encompasses a group of eye diseases that damage the optic nerve and can lead to vision loss. While medication is often the first line of defense, surgery is frequently required to lower IOP and prevent further damage. Traditional surgeries, such as trabeculectomy, create a new drainage pathway for fluid in the eye. However, these procedures can be more invasive and carry a higher risk of complications.
MIGS represents a newer generation of glaucoma surgeries. These techniques are typically less invasive than traditional surgery and aim to enhance the eye’s natural drainage system. Xen stents are small tubes implanted to create a new drainage pathway, while MIGS procedures encompass a range of techniques focusing on preserving the natural optic nerve function.
Frequently Asked questions about Glaucoma surgery
What are your thoughts on the evolving landscape of glaucoma surgery? Do you have concerns about potential complications? Share your perspectives in the comments below!
What are the primary mechanisms by which GDD implantation can lead to corneal edema?
Corneal Edema Risk Rises with glaucoma Drainage Device Use
Understanding Glaucoma Drainage Devices (gdds) and Corneal Health
Glaucoma drainage devices (GDDs), also known as glaucoma shunts, are surgically implanted devices used to lower intraocular pressure (IOP) in patients with glaucoma. While highly effective in managing complex glaucoma cases, a growing body of evidence highlights an increased risk of corneal edema – swelling of the cornea – following GDD implantation.This article delves into the mechanisms behind this risk, preventative measures, and management strategies. We’ll cover topics like tube shunt glaucoma, aqueous shunts, and the impact on corneal clarity.
Why gdds Can Lead to Corneal Edema
Several factors contribute to the development of corneal edema after GDD surgery. Understanding these mechanisms is crucial for both patients and ophthalmologists:
Hypotony: Over-filtration of aqueous humor, leading to excessively low IOP (hypotony), is a primary culprit. This can cause the cornea to swell due to decreased support. maintaining a target IOP range is vital.
Plate Malposition: If the baseplate of the GDD is positioned too anteriorly or is exposed, it can directly disrupt the corneal endothelium – the layer responsible for maintaining corneal clarity.Corneal endothelial cell loss is a meaningful concern.
Fibrosis and Inflammation: Post-operative inflammation and scar tissue formation (fibrosis) around the GDD can impede aqueous outflow and contribute to hypotony. Chronic inflammation also damages the endothelium.
Bleb-Related Issues: A filtering bleb, formed after surgery, can sometimes cause epithelial downgrowth onto the cornea, further compromising its clarity.
Aqueous Leak: Leakage of aqueous fluid from the tube can directly hydrate the cornea, leading to edema.
Identifying Corneal Edema: Symptoms and Diagnosis
Early detection is key to managing corneal edema effectively. Patients should be aware of the following symptoms:
Blurred Vision: A gradual decrease in visual acuity.
Halos Around Lights: Seeing rings around light sources, especially at night.
Light Sensitivity (Photophobia): Increased discomfort in bright light.
eye pain: Although not always present, some patients experience mild discomfort.
Corneal Haze: A cloudy or opaque appearance to the cornea.
Diagnosis involves a complete eye exam, including:
Slit-Lamp Biomicroscopy: Allows the ophthalmologist to visualize the cornea and identify edema.
Pachymetry: Measures corneal thickness. Increased thickness is indicative of edema.
Specular Microscopy: Counts the number of endothelial cells. A low cell density suggests endothelial dysfunction.
Confocal Microscopy: Provides high-resolution imaging of the corneal layers, aiding in the assessment of endothelial health.
Optical coherence Tomography (OCT): Can assess corneal thickness and identify structural changes.
management Strategies for Corneal Edema Post-GDD
Treatment options vary depending on the severity of the edema and the underlying cause.
- Conservative Management:
Topical Hypertonic Saline: draws fluid out of the cornea, temporarily improving clarity.
Bandage Contact Lenses: Provide a smooth refractive surface and reduce discomfort.
Artificial Tears: Lubricate the eye and alleviate symptoms.
- Surgical Interventions:
Baseplate Repositioning: If the baseplate is malpositioned, surgical repositioning can alleviate pressure on the endothelium.
Tube Revision/Manipulation: Adjusting the tube length or position can optimize aqueous outflow and reduce hypotony.
Endothelial Keratoplasty (DMEK/DSAEK): In severe cases with significant endothelial cell loss,corneal transplantation (specifically DMEK or DSAEK) might potentially be necessary to restore corneal clarity. DMEK surgery is often preferred due to its faster recovery and better visual outcomes.
Glaucoma Device Removal: In rare instances, removal of the GDD may be considered if other interventions fail.
Proactive Measures & Prevention
Preventing corneal edema is always preferable to treating it. Here are some proactive steps:
Careful Surgical Technique: Precise baseplate placement and meticulous surgical technique are paramount.
Post-Operative IOP Management: Close monitoring of IOP and prompt adjustment of medications to maintain a target range.
Anti-Inflammatory Regimen: Aggressive post-operative anti-inflammatory therapy to minimize fibrosis and inflammation.
Regular Follow-Up: Routine eye exams to monitor corneal health and