The Dawn of Hearing: How Ancient Fossils Are Rewriting Our Understanding of Mammalian Evolution
Imagine a world before whispers, before the rustle of leaves warned of predators, before the complex songs of birds filled the air. For centuries, scientists believed sophisticated hearing – the kind reliant on a middle ear – emerged relatively late in mammalian evolution. But a groundbreaking new study, centered around a 250-million-year-old fossil, suggests this crucial sense developed nearly 50 million years earlier than previously thought. This isn’t just paleontological trivia; it’s a fundamental shift in our understanding of how mammals, including ourselves, came to dominate the planet.
Unlocking the Secrets of Thrinaxodon liorhinus
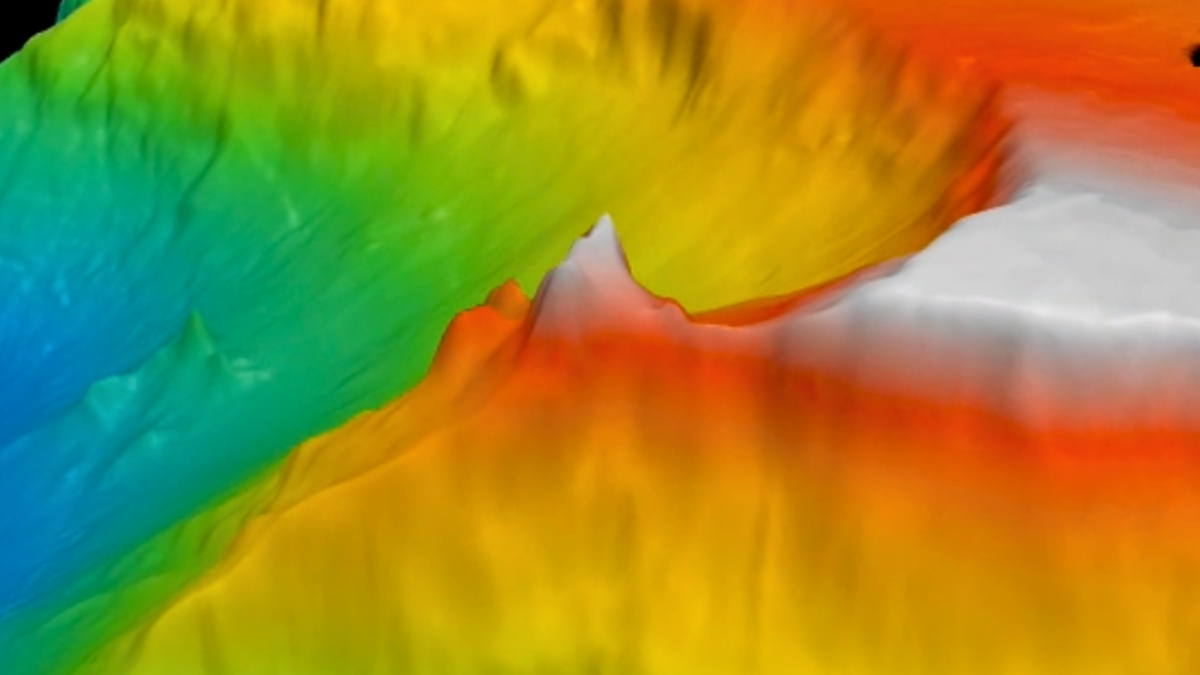
The key to this revelation lies within the skull and jaw of Thrinaxodon liorhinus, a cynodont – a mammal-like reptile that lived during the Early Triassic period, before the age of dinosaurs. Researchers at the University of Chicago employed cutting-edge computed tomography (CT) scans to create detailed 3D models of the fossil. These models weren’t just for visual inspection; they were used in engineering software typically reserved for stress-testing bridges and airplanes, allowing scientists to simulate how Thrinaxodon’s bones would react to different sound frequencies and pressures.
“We took a high-concept problem – that is, ‘how do ear bones wiggle in a 250-million-year-old fossil?’ – and tested a simple hypothesis using these sophisticated tools,” explains Alec Wilken, an evolutionary scientist at the University of Chicago. The results were startling. The simulations revealed that Thrinaxodon possessed an early form of an eardrum, capable of functioning effectively even without the fully detached middle-ear bones we associate with modern mammals.
From Bone Conduction to Tympanic Hearing: A Gradual Transition
Before the evolution of the middle ear, animals relied on bone conduction – sensing vibrations through their jawbones. This method is far less sensitive and precise than the tympanic hearing we experience today. The study suggests Thrinaxodon represented a pivotal transitional stage. Its eardrum, stretched across a hooked bone structure in its jaw, offered a significant upgrade over bone conduction, potentially enhancing its ability to locate prey, avoid predators, and even communicate.
Mammalian hearing evolution wasn’t a sudden leap, but a gradual refinement. Early cynodonts had ear bones attached to the jaw; over millions of years, these bones detached, forming the distinct middle ear of modern mammals. This decoupling allowed for greater amplification and directional hearing, giving mammals a crucial advantage in their environment.
The Role of Biomechanical Modeling
The success of this research hinges on the innovative application of biomechanical modeling. Previously, scientists relied on anatomical comparisons and speculation. Now, they can virtually “test” the hearing capabilities of extinct animals with unprecedented accuracy. This approach isn’t limited to hearing; it could be applied to study other aspects of ancient animal physiology, such as bite force or locomotion.
“Once we have the CT model from the fossil, we can take material properties from extant animals and make it as if our Thrinaxodon came alive,” says Zhe-Xi Luo, Wilken’s advisor. “That hasn’t been possible before, and this software simulation showed us that vibration through sound is essentially the way this animal could hear.”
Future Implications: Beyond Paleontology
This discovery has implications far beyond the realm of paleontology. Understanding the evolutionary origins of hearing can inform our understanding of hearing loss and disorders in modern mammals, including humans. For example, research into the genetic mechanisms that drove the detachment of the middle-ear bones could potentially lead to new therapies for conductive hearing loss.
Furthermore, the techniques used in this study could be applied to investigate the hearing capabilities of other extinct animals, shedding light on the evolution of communication and social behavior. Imagine being able to reconstruct the soundscape of the Cretaceous period, or understand how early whales evolved to hear underwater.
Did you know? The estimated hearing range of Thrinaxodon (38 to 1,243 hertz) was narrower than that of a healthy human (20 to 20,000 hertz), but still sufficient for detecting important sounds in its environment. Its sensitivity peaked at 1,000 hertz, a frequency range common in the vocalizations of many animals.
The Rise of Bio-Inspired Engineering
The principles underlying Thrinaxodon’s early hearing system could also inspire new technologies. Researchers are increasingly looking to nature for innovative solutions to engineering challenges – a field known as biomimicry. Could the design of Thrinaxodon’s eardrum lead to the development of more efficient or robust sound sensors? It’s a possibility worth exploring.
Pro Tip: When researching evolutionary biology, always consider the limitations of the fossil record. Fossils represent only a small fraction of the organisms that once lived, and interpreting their behavior and physiology requires careful analysis and creative thinking.
Frequently Asked Questions
Q: What is bone conduction?
A: Bone conduction is a method of hearing where sound vibrations are transmitted directly to the inner ear through the bones of the skull, bypassing the eardrum and middle ear. It’s less sensitive than tympanic hearing but was the primary way many early animals detected sound.
Q: How did researchers simulate Thrinaxodon’s hearing?
A: They created 3D models of the fossil’s skull and jaw and used engineering software designed to analyze vibrations in structures like bridges and airplanes. This allowed them to see how the bones would respond to different sound frequencies.
Q: What does this discovery tell us about the evolution of mammals?
A: It suggests that key features of mammalian hearing, like the eardrum, evolved much earlier than previously thought, potentially giving early mammals a competitive advantage.
Q: Could this research lead to new treatments for hearing loss?
A: Potentially. Understanding the genetic and developmental mechanisms behind the evolution of the middle ear could provide insights into the causes of hearing loss and inspire new therapeutic approaches.
As we continue to unearth the secrets of our ancient ancestors, we gain a deeper appreciation for the remarkable journey of life on Earth. The story of Thrinaxodon is a testament to the power of scientific curiosity and the enduring legacy of evolution. What new discoveries await us as we delve further into the fossil record?
Explore more insights on evolutionary biology in our comprehensive guide.