The Silent Threat After Surgery: How Cardiologist Collaboration Could Slash Post-Op Deaths
An estimated 4.2 million people die within 30 days of surgery worldwide each year. But what if a significant portion of those deaths weren’t inevitable, but preventable with a simple shift in post-operative care? A groundbreaking new study published in the European Heart Journal suggests that involving a cardiologist in the care of high-risk patients after surgery could dramatically reduce mortality and serious heart complications.
The Hidden Heart Risks of Non-Cardiac Surgery
We often think of heart surgery as the primary risk for cardiac events. However, even procedures like hip replacements or gallbladder removals can place immense stress on the cardiovascular system. Anesthesia, blood loss, inflammation, and fluctuating blood pressure all contribute to what doctors call perioperative myocardial infarction/injury (PMI) – damage to the heart muscle during or immediately after surgery. This often occurs without noticeable symptoms, particularly in patients aged 65 or older, or those with pre-existing heart or vascular conditions, affecting approximately 15% of high-risk individuals.
“PMI is a strong predictor for complications and death in the days and months after surgery,” explains Dr. Christian Puelacher of the University of Basel, Switzerland, lead author of the study. “It’s a silent threat that often goes undetected, leaving patients vulnerable.”
The Swiss Study: A ‘Natural Experiment’ in Cardiac Care
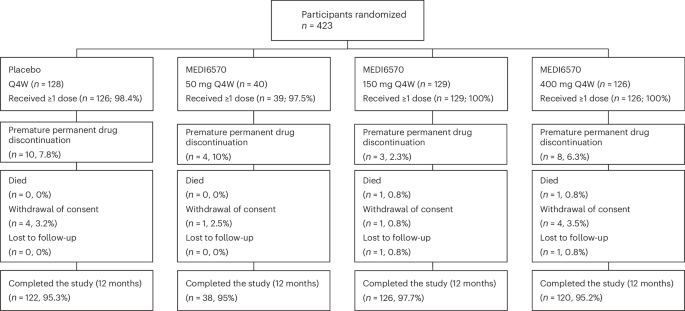
Researchers at the University of Basel and Cantonal Hospital Aarau, Switzerland, capitalized on a unique situation – variations in cardiologist availability – to investigate the impact of specialist cardiac evaluation. They analyzed data from 14,294 patients undergoing non-cardiac surgery, focusing on the 1,048 who showed signs of PMI based on troponin levels (a protein released when the heart is damaged).
Interestingly, 58.6% of these patients were evaluated by a cardiologist, while the remaining 41.4% weren’t – often due to factors like weekend or holiday staffing, or prioritization of urgent cases. This created a ‘natural experiment’ allowing researchers to compare outcomes between the two groups.
Significant Improvements with Cardiologist Involvement
The results were compelling. Patients who received a cardiologist evaluation were 35% less likely to die within a year of surgery and 46% less likely to experience serious heart problems like heart attack, heart failure, or dangerous irregular heart rhythms. They were also more likely to undergo heart imaging and receive stronger medications.
Expert Insight: “Our study shows that having a cardiologist involved in a patient’s care after PMI is associated with fewer serious heart problems and better survival one year later,” says Dr. Puelacher. “These findings underscore the importance of close teamwork between surgical and heart teams to optimize patient outcomes.”
Looking Ahead: The Rise of Proactive Cardiac Monitoring
While this study demonstrates a strong association, it’s crucial to remember it doesn’t prove cause-and-effect. As Dr. Noemi Glarner, a co-author of the study, points out, a randomized controlled trial is needed to definitively confirm these results. However, the evidence is compelling enough to warrant a shift in practice.
We’re already seeing this shift in action. The researchers are currently implementing PMI screening programs in hospitals across Switzerland and Austria. But this is just the beginning. The future of post-operative care will likely involve:
- Widespread PMI Screening: Routine troponin testing after non-cardiac surgery will become standard practice, particularly for high-risk patients.
- AI-Powered Risk Stratification: Artificial intelligence algorithms will analyze patient data to identify those at highest risk of PMI, allowing for targeted interventions.
- Telecardiology Integration: Remote cardiologist consultations via telehealth will expand access to specialist care, especially in rural areas or during off-hours.
- Enhanced Collaboration Protocols: Hospitals will develop clear protocols for seamless communication and collaboration between surgical and cardiology teams.
The Impact of an Aging Population and Increasing Surgical Volume
The need for these changes is becoming increasingly urgent. As the global population ages, the volume of surgeries is steadily rising. This means more patients will be at risk of PMI, and the potential impact of improved post-operative cardiac care will be even greater.
Did you know? The number of surgeries performed globally is projected to increase by 70% by 2030, according to a report by the World Health Organization.
Beyond PMI: A Holistic Approach to Perioperative Cardiac Care
The focus shouldn’t solely be on detecting and treating PMI. A holistic approach to perioperative cardiac care will also involve:
- Pre-operative Cardiac Optimization: Identifying and managing pre-existing heart conditions before surgery.
- Minimally Invasive Surgical Techniques: Reducing the physiological stress of surgery through less invasive procedures.
- Personalized Anesthesia Protocols: Tailoring anesthesia regimens to minimize cardiovascular impact.
Pro Tip: If you are scheduled for non-cardiac surgery, especially if you have pre-existing heart conditions or are over 65, discuss your risk factors with your doctor and ask about post-operative cardiac monitoring.
Frequently Asked Questions
Q: What is PMI and why is it dangerous?
A: PMI, or perioperative myocardial infarction/injury, is damage to the heart muscle that occurs during or immediately after surgery. It’s often silent, meaning it doesn’t cause noticeable symptoms, but it significantly increases the risk of complications and death.
Q: Who is at risk of PMI?
A: High-risk patients include those aged 65 or older, individuals with pre-existing heart or vascular disease, and those undergoing complex or lengthy surgeries.
Q: What can be done to prevent PMI?
A: Pre-operative cardiac optimization, minimally invasive surgical techniques, personalized anesthesia, and post-operative cardiac monitoring with cardiologist involvement can all help reduce the risk of PMI.
Q: Is a cardiology consult always necessary after surgery?
A: While not always necessary, a cardiology consult is strongly recommended for high-risk patients who show signs of PMI based on troponin levels.
The study from the University of Basel provides a crucial piece of the puzzle in improving post-operative outcomes. As healthcare systems embrace proactive cardiac monitoring and collaborative care models, we can expect to see a significant reduction in preventable deaths and a brighter future for patients undergoing surgery. What are your thoughts on the role of AI in predicting and preventing PMI? Share your insights in the comments below!
Explore more insights on cardiovascular health and preventative care on Archyde.com.