Your Biological Age Isn’t a Number – It’s a Trajectory, and It’s Changing How We Detect Disease
Imagine a future where a simple annual check-up doesn’t just tell you if you’re developing a disease, but when – years, even decades, before symptoms appear. That future is closer than you think. New research leveraging the power of “lifecycle clocks” built from millions of patient records reveals that aging isn’t a series of distinct stages, but a continuous, measurable physiological trajectory. This isn’t just about living longer; it’s about radically extending healthspan – the years lived in good health.
The Rise of the ‘Full-Lifecycle Clock’
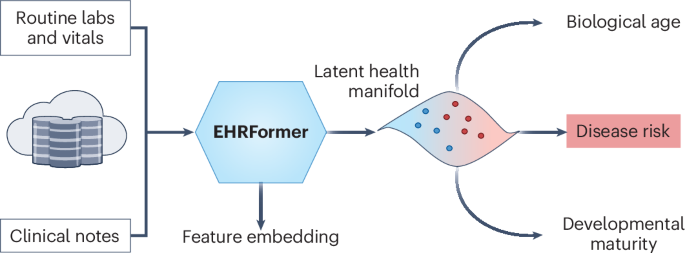
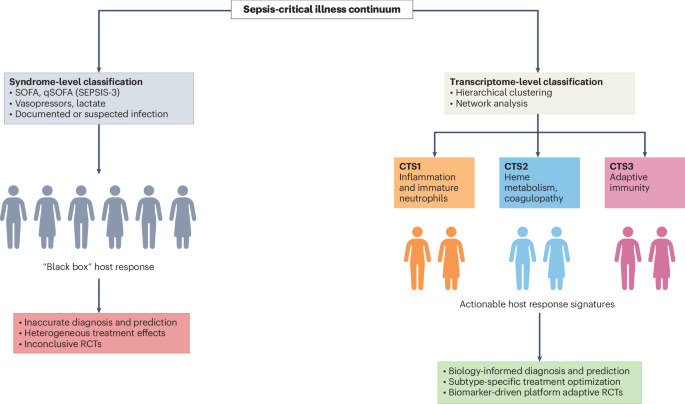
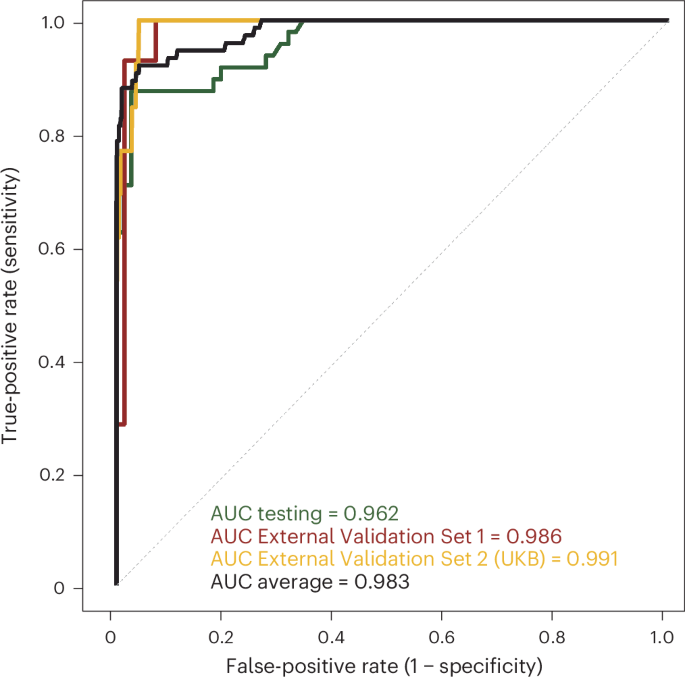
Traditionally, aging research has focused on identifying biomarkers associated with specific age-related diseases. However, a study published in Nature Medicine demonstrates a more holistic approach. Researchers have developed a sophisticated clock, trained on an unprecedented dataset of routine clinical records, that maps the entire human lifespan – from development through aging – as a single, interconnected process. This biological age clock isn’t simply based on chronological age; it’s based on how your body actually functions, measured through a vast array of clinical data points.
“What’s remarkable is the scale,” explains Dr. Morgan Levine, a leading researcher in the field of epigenetic aging (and not directly involved in this study, but a key voice in the space). “Previous aging clocks were often built on smaller, more focused datasets. This new clock’s power comes from its ability to integrate information from millions of individuals, providing a far more accurate and nuanced picture of the aging process.” Learn more about Dr. Levine’s work here.
Early Disease Detection: A Paradigm Shift
The implications for early disease detection are profound. Because the lifecycle clock establishes a baseline of ‘normal’ physiological progression, deviations from that trajectory can signal the onset of disease long before traditional diagnostic methods. This is particularly exciting for conditions like cardiovascular disease, Alzheimer’s, and certain cancers, where early intervention is critical.
Predicting Risk, Personalizing Prevention
Instead of waiting for symptoms, doctors could use these clocks to identify individuals at increased risk and implement personalized preventative strategies. Imagine a scenario where a slight acceleration in your biological aging trajectory flags a predisposition to type 2 diabetes. Lifestyle interventions – diet, exercise, stress management – could be implemented proactively, potentially delaying or even preventing the disease’s onset. This moves healthcare from reactive treatment to proactive prevention.
Beyond Detection: Unlocking the Mechanisms of Aging
This research isn’t just about predicting disease; it’s about understanding the fundamental mechanisms that drive aging itself. By analyzing the patterns and correlations within the lifecycle clock data, scientists can gain insights into the biological processes that contribute to age-related decline. This knowledge can then be used to develop targeted interventions aimed at slowing down or even reversing the aging process.
The Role of ‘Geroscience’
This aligns with the growing field of ‘geroscience’ – the study of the biological mechanisms of aging – which posits that targeting the fundamental processes of aging can have broad benefits across multiple age-related diseases. Interventions like senolytics (drugs that clear senescent cells) and caloric restriction mimetics are examples of geroscience-based approaches currently under investigation. The lifecycle clock provides a powerful tool for evaluating the effectiveness of these interventions.
Future Trends: AI, Wearables, and the Quantified Self
The future of lifecycle clocks is inextricably linked to advancements in artificial intelligence and wearable technology. As AI algorithms become more sophisticated, they will be able to analyze even more complex datasets and identify subtle patterns that would be impossible for humans to detect. Wearable sensors, continuously monitoring physiological data like heart rate variability, sleep patterns, and activity levels, will provide a constant stream of real-time information, further refining the accuracy of these clocks.
We’re moving towards a future where individuals have access to their own personalized lifecycle clocks, empowering them to take control of their health and make informed decisions about their lifestyle. This ‘quantified self’ movement, combined with the power of AI-driven insights, has the potential to revolutionize healthcare as we know it.
The development of these full-lifecycle clocks represents a fundamental shift in how we understand and approach aging. It’s no longer about simply adding years to life, but about adding life to years. What are your predictions for the impact of this technology on healthcare? Share your thoughts in the comments below!