The Body Clock and Cancer Care: Why Time of Day May Be the Next Frontier in Immunotherapy
For decades, cancer treatment has focused on what drugs to use and how to administer them. But a growing body of research suggests we’ve been overlooking a critical variable: when. Emerging evidence reveals that the body’s natural circadian rhythms – the internal clocks governing nearly all biological processes – profoundly influence the effectiveness of cancer immunotherapy, potentially explaining why some patients respond dramatically while others don’t. This isn’t just about optimizing schedules; it’s about aligning treatment with the body’s natural defenses, and it’s poised to reshape how we approach cancer care.
The Circadian Rhythm-Immune System Connection
Our immune system doesn’t operate at a constant level throughout the day. Key immune cells, like cytotoxic CD8+ T cells – the soldiers that directly attack cancer cells – exhibit daily fluctuations in their activity, trafficking, and ability to infiltrate tumors. These rhythms are regulated by the circadian clock, a complex network of genes and proteins found in nearly every cell. Studies, including those highlighted by Fortin et al. (2024) in Nature Immunology, demonstrate that disrupting these rhythms can significantly impair the anti-tumor immune response. Essentially, giving immunotherapy when the immune system is ‘asleep’ may render it far less effective.
Evidence Mounts: Timing Matters for Immunotherapy
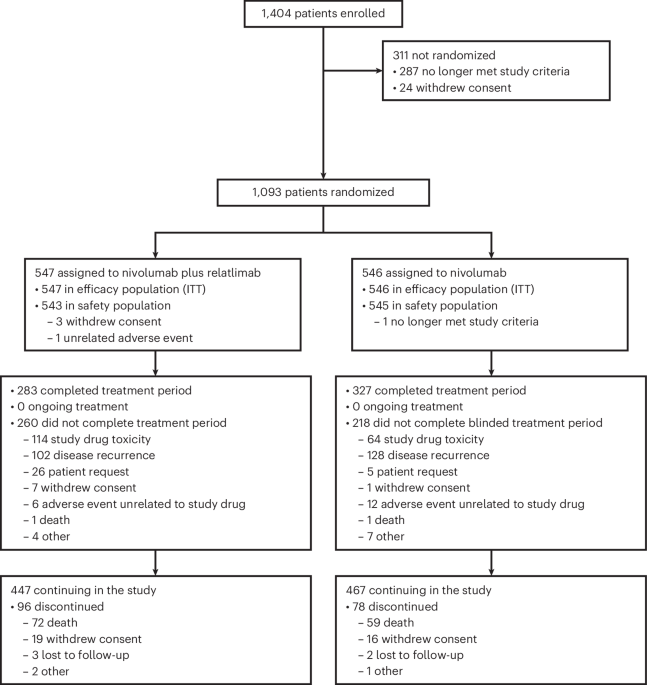
The initial observations came from studies looking at melanoma patients. Qian et al. (2021), publishing in The Lancet Oncology, found that patients receiving immunotherapy in the afternoon showed significantly longer overall survival compared to those treated in the morning. This wasn’t an isolated finding. Subsequent research has extended these observations to other cancers, including renal cell carcinoma (Patel et al., 2024, Journal of Immunotherapy Cancer), head and neck cancer (Ruiz-Torres et al., 2024, Oral Oncology), and non-small cell lung cancer (NSCLC) – the focus of much recent investigation. Hirata et al. (2024) even reported preliminary findings suggesting a link between infusion timing and outcomes in locally advanced NSCLC, published in the JTO Clinical Research Reports.
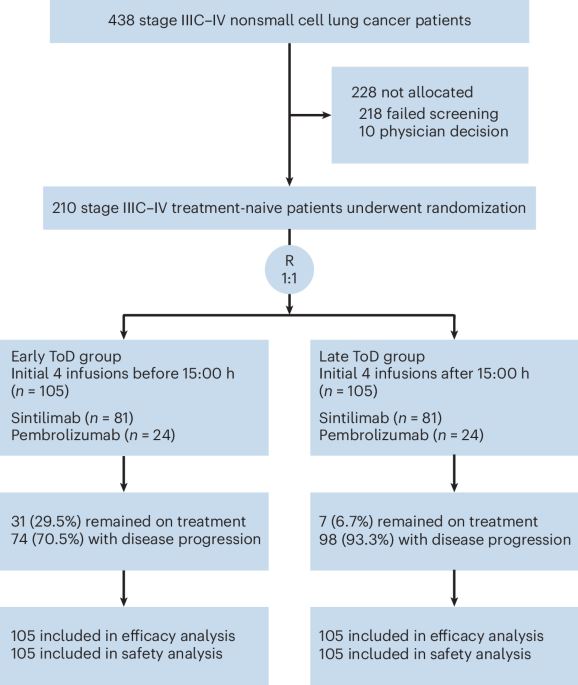
Non-Small Cell Lung Cancer: A Deep Dive into Timing
Non-small cell lung cancer is a particularly compelling area of study. The interplay between chemotherapy, immune checkpoint inhibitors, and circadian rhythms is complex. Huang et al. (2025, EBioMedicine) recently published a bicontinental study showing that the time of day of combined immuno-chemotherapy correlated with overall survival. While the optimal timing remains debated – Cortellini et al. (2022, Annals of Oncology) cautioned against prematurely advocating for morning infusions – the consensus is growing that timing is a crucial factor. This is further complicated by the fact that individual circadian rhythms can vary significantly, influenced by genetics, lifestyle, and even geographic location.
Beyond Infusion Time: Considering the Patient’s Internal Clock
The emerging field of ‘chronotherapy’ goes beyond simply scheduling infusions. It aims to personalize treatment based on an individual’s chronotype – whether they are a ‘morning person’ or a ‘night owl’ – and their unique circadian profile. Researchers are exploring ways to measure these profiles and tailor treatment schedules accordingly. Furthermore, factors like fasting and meal timing are also being investigated for their potential to enhance immunotherapy efficacy, as suggested by Vilalta et al. (2021) in a presentation at the European Society for Medical Oncology (ESMO) Congress.
The Role of T Cell Dynamics and Biomarkers
Understanding why timing matters is crucial. Wang et al. (2024, Cell) demonstrated that circadian rhythms directly influence the infiltration and function of CD8+ T cells within tumors. This is linked to the expression of specific genes regulated by the circadian clock. Identifying biomarkers that predict an individual’s response to immunotherapy based on their circadian profile is a major research priority. Miao et al. (2022, Frontiers in Immunology) and Wang et al. (2023, Journal of Thoracic Disease) have shown that specific T lymphocyte subsets can predict immunotherapy efficacy, potentially offering clues for personalized timing strategies.
Future Directions and Clinical Implications
The implications of this research are far-reaching. We may see a shift towards more personalized immunotherapy schedules, incorporating chronotype assessment and potentially even interventions to ‘reset’ disrupted circadian rhythms. Clinical trials are needed to definitively establish the optimal timing for different immunotherapies and cancer types. Furthermore, integrating circadian considerations into the design of new immunotherapeutic agents could lead to more effective treatments. The National Comprehensive Cancer Network (NCCN) guidelines (Riely et al., 2024) are beginning to acknowledge the importance of these factors, signaling a growing awareness within the medical community.
The future of cancer immunotherapy isn’t just about finding new drugs; it’s about understanding the intricate interplay between those drugs and the body’s natural rhythms. By harnessing the power of the circadian clock, we may unlock a new era of personalized and effective cancer care. What steps will oncologists take to incorporate these findings into their practice? Share your thoughts in the comments below!