Long COVID Risk Doubles with Reinfection in Children: What the Future Holds
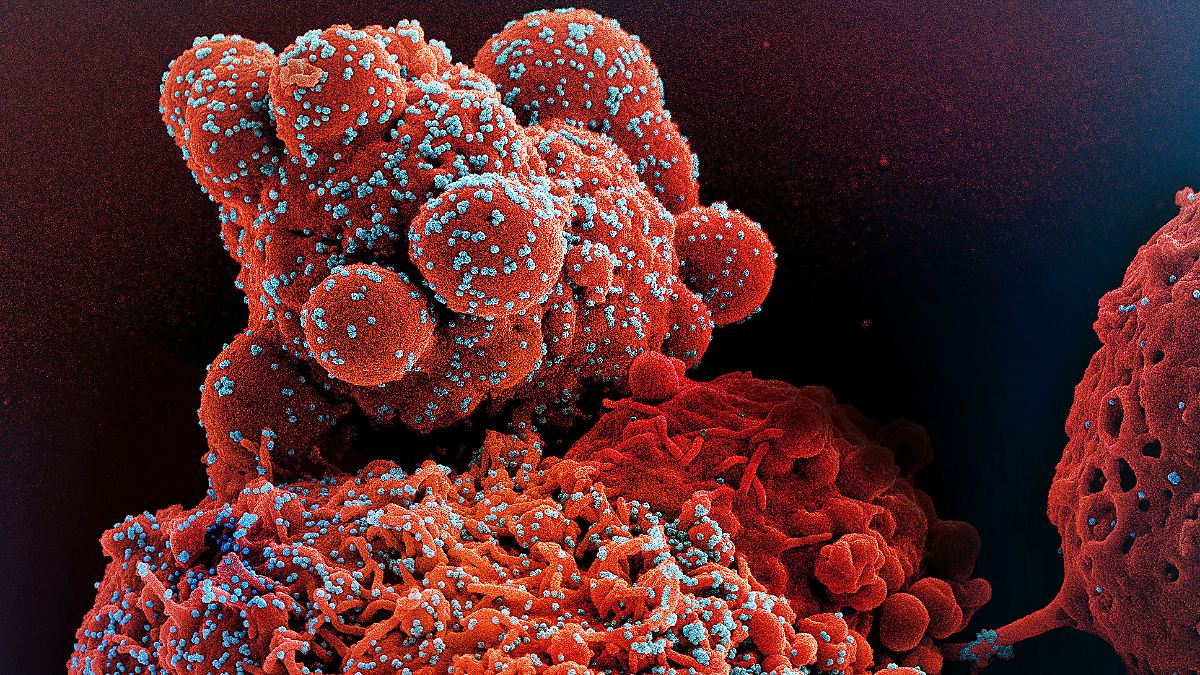
Nearly one in 500 children experienced long COVID symptoms after a second documented COVID-19 infection, according to groundbreaking research. This startling statistic, more than double the rate following an initial infection, underscores a growing concern: repeated exposure to SARS-CoV-2 isn’t just causing more cases, it’s significantly increasing the risk of debilitating long-term health issues in young people. But what does this mean for the future of pediatric healthcare, and what can parents and policymakers do to mitigate the escalating threat?
The Reinfection Risk: A Deep Dive into the Lancet Study
The study, published in The Lancet Infectious Diseases, analyzed health records of over 460,000 children and adolescents across 40 US pediatric hospitals between January 2022 and October 2023 – a period heavily influenced by the Omicron variant and its subvariants. Researchers meticulously compared health outcomes after first and second infections, revealing a concerning trend. While approximately 904 children per million developed long COVID within six months of their first infection, that number surged to 1,884 per million after reinfection. This isn’t simply a linear increase; it represents a doubling of risk, highlighting the cumulative impact of repeated viral exposure.
Beyond Fatigue: The Spectrum of Long COVID Symptoms
Long COVID in children isn’t a single illness; it’s a complex constellation of symptoms. The Lancet study identified a range of persistent conditions linked to reinfection, including heart inflammation (myocarditis), blood clots, kidney injury, cognitive difficulties, debilitating fatigue, and respiratory problems. These aren’t minor inconveniences; they can significantly disrupt a child’s development, education, and overall quality of life. The multisystem nature of these effects emphasizes the virus’s ability to impact multiple organ systems, even in seemingly mild cases.
Long COVID isn’t just a post-viral syndrome; it’s a potential chronic illness demanding urgent attention.
Future Trends: What’s on the Horizon?
Several key trends are likely to shape the future of pediatric long COVID:
1. The Cumulative Impact of Repeated Infections
As SARS-CoV-2 continues to evolve and immunity wanes, reinfections are becoming increasingly common. The study suggests that each subsequent infection may further elevate the risk of long COVID, potentially leading to a cumulative burden of morbidity. This raises the specter of a generation grappling with chronic health issues stemming from repeated viral exposures. We may see a rise in the prevalence of multi-system inflammatory syndrome in children (MIS-C) and other post-viral complications.
2. The Role of Vaccination and Prior Immunity
While the study didn’t specifically analyze the impact of vaccination status on reinfection risk, experts emphasize that vaccines remain the most effective tool for preventing both initial infections and reinfections. However, the effectiveness of current vaccines against new variants is constantly evolving. Future vaccine development may focus on broader-spectrum immunity and improved durability, potentially reducing the risk of both acute infection and long COVID. Understanding how prior infection and vaccination interact to influence long COVID risk will be crucial.
3. Emerging Diagnostic and Therapeutic Approaches
Currently, diagnosing long COVID is challenging, relying heavily on symptom reporting and excluding other potential causes. Researchers are actively seeking biomarkers – measurable indicators in the blood or other bodily fluids – that can objectively identify long COVID and differentiate it from other conditions. Furthermore, clinical trials are underway to evaluate potential treatments, ranging from antiviral therapies to immunomodulatory drugs. Personalized medicine approaches, tailoring treatment to individual patient characteristics, may become increasingly important.
Actionable Insights for Parents and Policymakers
Addressing the growing threat of pediatric long COVID requires a multi-faceted approach:
For Parents:
- Prioritize Vaccination: Ensure your children are up-to-date on their COVID-19 vaccinations and boosters.
- Layered Protection: Encourage mask-wearing in crowded indoor settings, especially during periods of high transmission.
- Early Intervention: If your child develops persistent symptoms after a COVID-19 infection, seek medical attention promptly.
- Advocate for Your Child: Be persistent in seeking answers and support from healthcare providers.
For Policymakers:
- Invest in Research: Increase funding for research into the causes, diagnosis, and treatment of long COVID in children.
- Strengthen Public Health Infrastructure: Improve surveillance systems to track the incidence and prevalence of long COVID.
- Expand Access to Care: Ensure that all children have access to affordable and comprehensive healthcare, including specialized long COVID clinics.
- Promote Vaccination Equity: Address disparities in vaccination rates to protect vulnerable populations.
Frequently Asked Questions
Q: Is long COVID in children as severe as in adults?
A: While the symptoms can overlap, long COVID in children often presents differently than in adults. Children may be more likely to experience cognitive difficulties, fatigue, and respiratory problems, while adults may be more prone to cardiovascular complications. The long-term consequences are still being studied.
Q: What can be done to help a child with long COVID?
A: Management of long COVID symptoms is often individualized and may involve physical therapy, cognitive behavioral therapy, medication to manage specific symptoms, and supportive care. A multidisciplinary approach is often most effective.
Q: Are new variants of COVID-19 increasing the risk of long COVID?
A: The relationship between specific variants and long COVID risk is still being investigated. However, the increased transmissibility of newer variants like Omicron and its subvariants means more people are getting infected, and therefore, more people are at risk of developing long COVID.
The escalating risk of long COVID following reinfection in children demands a proactive and comprehensive response. By prioritizing vaccination, investing in research, and expanding access to care, we can mitigate the long-term consequences of this evolving pandemic and protect the health and well-being of future generations. What steps will you take to safeguard your family and advocate for change in your community?