Basketball Star Achille Polonara Overcomes Health Crisis Following Bone Marrow Transplant
Table of Contents
- 1. Basketball Star Achille Polonara Overcomes Health Crisis Following Bone Marrow Transplant
- 2. near-Fatal Complications arise Post-Transplant
- 3. A moment of Relief and Party
- 4. Battling Leukemia and a History of Illness
- 5. Road to Recovery and Future Outlook
- 6. Understanding Bone Marrow Transplants and Leukemia
- 7. Frequently Asked questions
- 8. What are the potential long-term cognitive and physical effects someone might experience after recovering from a coma, as highlighted in the text?
- 9. Achille Polonara Recounts Near-Death Experience: “In Coma for Ten Days, Told I’d Die but Now Leaving hospital”
- 10. The Shocking health Crisis of Achille Polonara
- 11. details of Polonara’s Condition & Initial Diagnosis
- 12. The Ten Days in a Coma: A Critical Period
- 13. The Remarkable Turnaround & Recovery Process
- 14. Athlete Health & sudden Illness: A Growing Concern
- 15. What’s Next for Achille Polonara?
- 16. Understanding Coma Recovery & Long-Term Effects
- 17. The Role of Early Diagnosis & Intervention
After a harrowing battle with leukemia and a recent critical health setback, professional basketball player achille Polonara has demonstrated remarkable resilience, leaving the hospital temporarily to celebrate a personal milestone.
near-Fatal Complications arise Post-Transplant
Previously undergoing a bone marrow transplant in September, Achille Polonara experienced a severe downturn in his condition in recent weeks, ultimately leading to a coma.
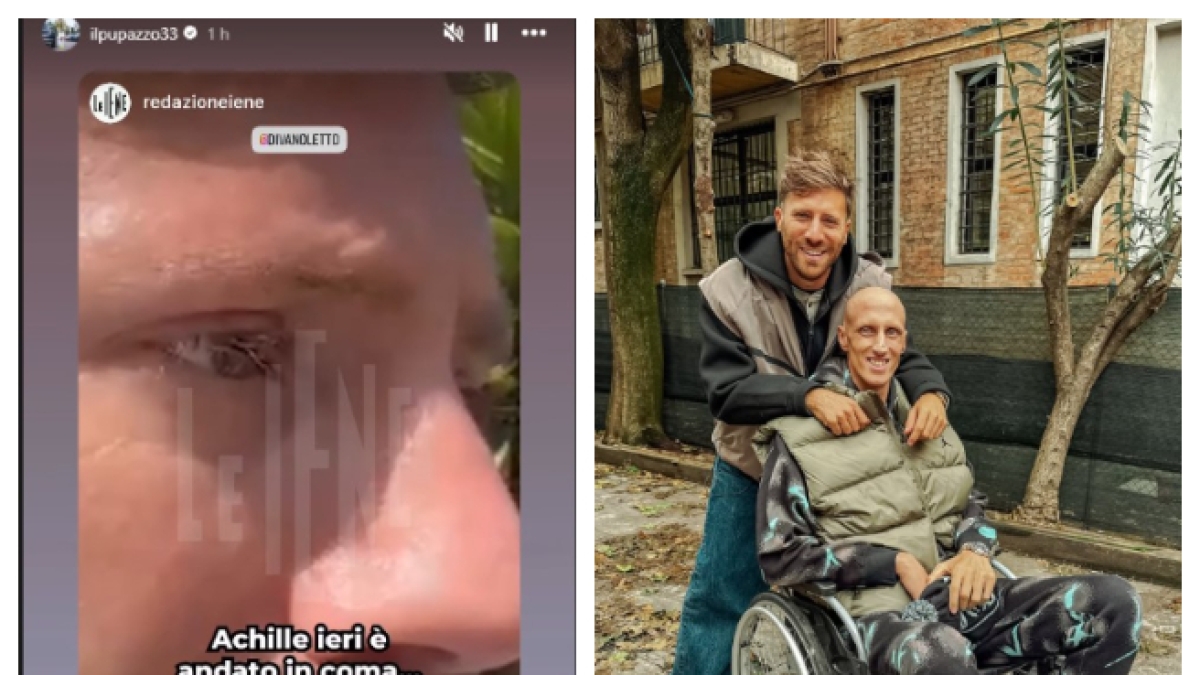
The alarming development was revealed by his wife, Erika Bufano, during an interview on the Italian television program, “Le Iene.”
According to Bufano, Polonara developed a blood clot that triggered a critical lack of oxygen to his brain, putting his life at serious risk.
A moment of Relief and Party
Fortunately, Polonara’s condition gradually improved, and he was briefly discharged from the hospital over the weekend to celebrate the fifth birthday of his daughter, Vitoria.
This temporary release represents a meaningful step in his recovery journey and a much-needed moment of joy for the family.
Polonara himself acknowledged the gravity of his situation, expressing gratitude for being alive and regaining his health.
“They told me that 90% of the time I would die,” he stated, “I don’t remember much, it’s as if I slept. Being able to breathe some fresh air again was a great feeling.”
Battling Leukemia and a History of Illness
Polonara’s current struggle follows a previous battle with testicular neoplasia two years ago.
The recent diagnosis of acute myeloid leukemia disrupted his career with Virtus Bologna, requiring immediate hospitalization during the championship finals.
Throughout his treatment, Polonara has demonstrated unbelievable strength, with colleagues and friends offering unwavering support.
He underwent chemotherapy cycles, and received a bone marrow transplant from a compatible donor located in America.
Road to Recovery and Future Outlook
While Polonara’s recovery continues with ongoing checks and rehabilitation at Saint Ursula Hospital, doctors are optimistic about his progress.
He is expected to gradually increase his time outside the hospital, with the ultimate goal of a full return to health.
Polonara remains hopeful and determined to overcome this challenge,buoyed by the love and support of his family,friends,and colleagues.
Understanding Bone Marrow Transplants and Leukemia
Bone marrow transplants, also known as stem cell transplants, are a crucial treatment option for various cancers, including leukemia.
The procedure involves replacing damaged bone marrow with healthy stem cells, allowing the body to produce new, healthy blood cells.
Leukemia, a cancer of the blood and bone marrow, hinders the body’s ability to fight infection.Various types exist, requiring tailored treatment approaches.
American Cancer Society provides thorough data on leukemia and bone marrow transplants.
Frequently Asked questions
- What is a bone marrow transplant? A medical procedure to replace damaged bone marrow with healthy stem cells.
- What is leukemia? A cancer affecting blood and bone marrow, preventing proper blood cell production.
- What are the common side effects of a bone marrow transplant? Potential side effects include infection, fatigue, and graft-versus-host disease.
- How long does it take to recover from a bone marrow transplant? Recovery can take months to years, varying based on individual circumstances.
- What is acute myeloid leukemia? A fast-growing cancer of the blood and bone marrow.
What are the potential long-term cognitive and physical effects someone might experience after recovering from a coma, as highlighted in the text?
Achille Polonara Recounts Near-Death Experience: “In Coma for Ten Days, Told I’d Die but Now Leaving hospital”
The Shocking health Crisis of Achille Polonara
Italian basketball player Achille Polonara, currently with Virtus Segafredo Bologna, recently faced a harrowing health scare that left him in a coma for ten days. News broke on November 5th, 2025, that Polonara was informed he might not survive, yet remarkably, he is now preparing to leave the hospital. This story has sent ripples through the European basketball community and beyond,prompting discussions about sudden health issues in athletes and the power of recovery.
details of Polonara’s Condition & Initial Diagnosis
while the exact nature of Polonara’s illness remains somewhat private, initial reports indicate a severe inflammatory condition affecting multiple organs. Sources close to the player revealed that he experienced a rapid deterioration in health, leading to immediate hospitalization and subsequent induction into a medically-induced coma.
* Rapid Onset: The illness struck quickly, catching both Polonara and his medical team off guard.
* Multi-Organ Impact: the inflammation wasn’t isolated, impacting several vital organs and creating a critical situation.
* Medically Induced Coma: Doctors opted for a medically induced coma to allow Polonara’s body to rest and fight the inflammation.
* Grim Prognosis: During the most critical phase, medical professionals reportedly informed his family that the chances of survival were extremely low.
The Ten Days in a Coma: A Critical Period
The ten days Polonara spent in a coma were a period of intense anxiety for his family,teammates,and fans. A coma, defined as a prolonged state of unconsciousness, requires intensive care and constant monitoring. During this time, the body’s functions are supported artificially, and the focus is on stabilizing the patient and allowing the underlying condition to resolve.
The medical team focused on:
- Controlling Inflammation: Utilizing medications to reduce the widespread inflammation.
- Organ Support: Providing mechanical ventilation and other life support measures to assist failing organs.
- Neurological Monitoring: Closely tracking brain activity to assess neurological function.
The Remarkable Turnaround & Recovery Process
against all odds, Polonara began to show signs of improvement. The inflammation gradually subsided, and his organs started to regain function. He was slowly brought out of the coma, and after a period of observation and rehabilitation, he is now deemed well enough to leave the hospital.
* gradual Improvement: The recovery wasn’t immediate; it was a slow and steady process.
* Rehabilitation Focus: Polonara will require ongoing rehabilitation to regain his strength and physical conditioning. This will likely include physiotherapy, cardiovascular training, and a carefully managed return to basketball-specific drills.
* Emotional Support: The psychological impact of such a near-death experience is important, and Polonara will likely benefit from emotional support and counseling.
Athlete Health & sudden Illness: A Growing Concern
Polonara’s case highlights the vulnerability of even elite athletes to sudden and severe health issues. While athletes are generally known for their physical fitness, they are not immune to underlying medical conditions or unexpected complications.
* Hypertrophic Cardiomyopathy: A common concern in athletes, involving thickening of the heart muscle.
* Sudden Cardiac Arrest: although rare, a perhaps fatal event that can occur during or after exercise.
* Inflammatory Conditions: Autoimmune diseases and other inflammatory conditions can affect athletes of all levels.
* Importance of Regular check-ups: Comprehensive medical screenings are crucial for identifying potential health risks in athletes.
What’s Next for Achille Polonara?
While a full return to professional basketball is not yet guaranteed, Polonara’s positive progress is incredibly encouraging. He will continue to work closely with his medical team to monitor his health and gradually rebuild his physical condition. The timeline for his return to the court remains uncertain, but his determination and the support of his team and fans will undoubtedly play a vital role in his recovery. Virtus Segafredo Bologna has expressed unwavering support for Polonara, emphasizing that his health is the top priority.
Understanding Coma Recovery & Long-Term Effects
Recovering from a coma is a complex process with varying outcomes. The length of time spent in a coma, the underlying cause, and the individual’s overall health all influence the recovery trajectory. Potential long-term effects can include:
* Cognitive Impairment: Difficulties with memory, attention, and problem-solving.
* Physical Disabilities: Weakness,paralysis,or difficulty with coordination.
* Speech and Language Problems: Difficulty communicating effectively.
* Emotional and Behavioral Changes: Anxiety, depression, or irritability.
Specialized rehabilitation programs are essential for maximizing recovery and addressing these potential challenges.
The Role of Early Diagnosis & Intervention
In cases of severe