“`html
National Sickle Cell Awareness Month: Understanding the Disease and New Hope for Treatment
Table of Contents
- 1. National Sickle Cell Awareness Month: Understanding the Disease and New Hope for Treatment
- 2. What is Sickle Cell disease?
- 3. Key Statistics on Sickle Cell Disease
- 4. Sickle Cell Trait Versus Sickle Cell Disease: A Crucial Distinction
- 5. The Spectrum of Complications Associated with Sickle Cell Disease
- 6. Evolving Treatment Strategies for Sickle Cell Disease
- 7. Established and Emerging Therapies
- 8. Navigating Financial Assistance for Sickle Cell Disease Care
- 9. The Lifesaving Role of Blood Donations
- 10. Early Detection: The Key to Effective Management
- 11. Living Fully with Sickle Cell disease
- 12. Understanding Sickle Cell Disease Over Time
- 13. Frequently Asked Questions About Sickle Cell Disease
- 14. What are the genetic requirements for a child to be diagnosed with sickle cell disease?
- 15. Navigating Sickle Cell Disease: Your Complete Guide for National Sickle Cell Awareness Month 2025
- 16. Understanding Sickle Cell Disease: The basics
- 17. What Causes Sickle Cell Disease?
- 18. Recognizing the Symptoms of Sickle Cell disease
- 19. Diagnosis and Testing for Sickle Cell Disease
- 20. Managing Sickle Cell Disease: Treatment Options
- 21. current Treatment Approaches
- 22. Emerging therapies & Potential Cures
- 23. Living with Sickle Cell Disease: Practical Tips & Support
- 24. Benefits of Early Intervention and Consistent Care
As National Sickle Cell Awareness Month begins, attention is focused on the urgent need for increased research, improved treatment options, and comprehensive support for the approximately 100,000 Americans living with sickle cell disease (SCD). This year’s “Sickle Cell Matters 2025” campaign underscores the vital importance of public awareness regarding this often-misunderstood inherited condition.
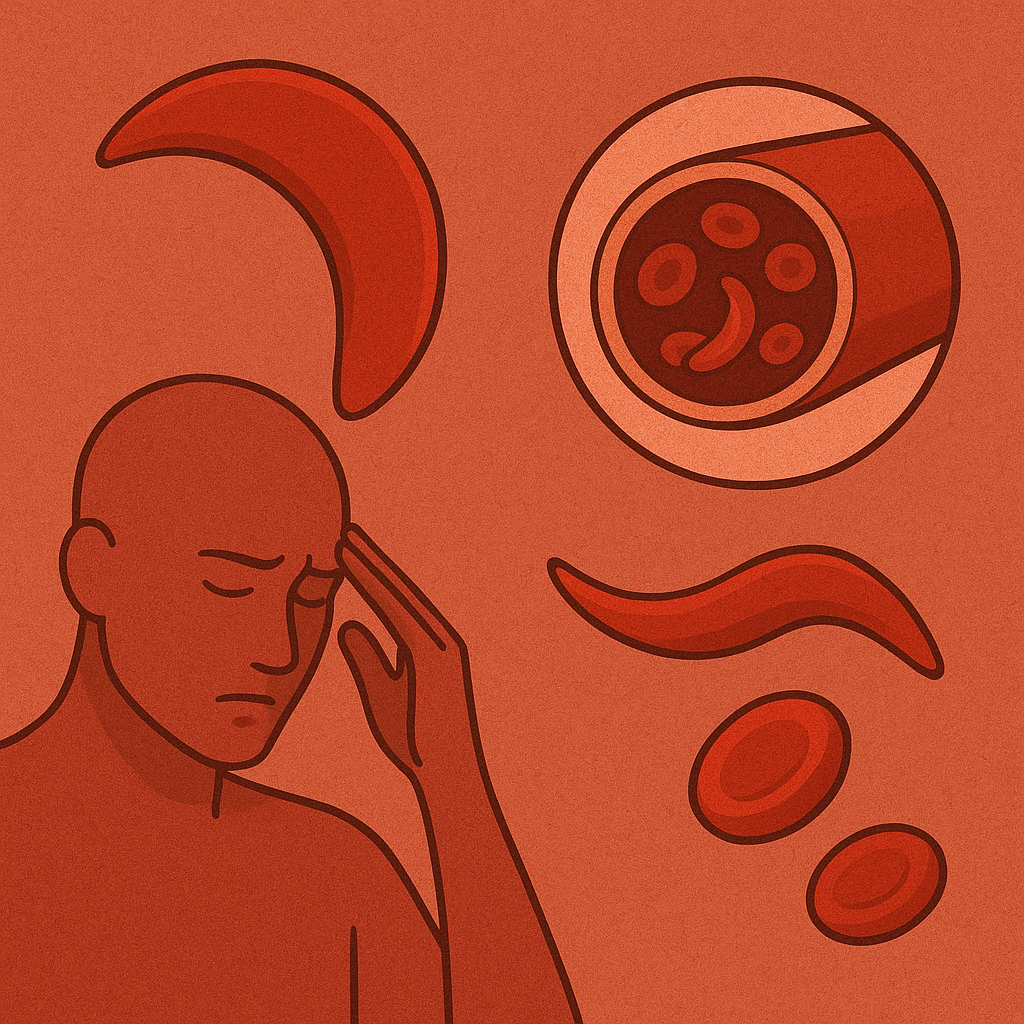
What is Sickle Cell disease?
Sickle cell disease represents the most prevalent inherited blood disorder in the United states. It encompasses a spectrum of genetic conditions that alter the shape of red blood cells, transforming them from their normal, pliable round form into a rigid, crescent-like shape-resembling a farm tool, a sickle.These abnormally shaped cells contain a defective form of hemoglobin, known as hemoglobin S, leading to a cascade of potential health complications throughout the body.
Key Statistics on Sickle Cell Disease
The impact of sickle cell disease is significant, particularly within specific populations. The following data highlights the scope of the condition:
| Population Group | Estimated Affected Individuals (US) | Incidence Rate (Births) |
|---|---|---|
| Non-Hispanic Black or African American | ~90,000 | 1 in 365 |
| hispanic or Latino | ~3,000 – 9,000 | 1 in 16,300 |
| Worldwide | >500,000 newborns annually | Varies significantly by region |
Source: Data compiled from various health organizations as of September 2025.
Sickle Cell Trait Versus Sickle Cell Disease: A Crucial Distinction
It is imperative to differentiate between sickle cell trait and sickle cell disease.Millions of individuals carry sickle cell trait, often without exhibiting any health problems. However, when both parents possess the trait, each pregnancy carries a 25% probability of resulting in a child born with sickle cell disease. Genetic counseling is essential for prospective parents considering family planning.
The Spectrum of Complications Associated with Sickle Cell Disease
Sickle cell disease can trigger a wide range of medical challenges, impacting numerous organs and systems. Some of the most common and severe complications include:
- Pain Crises (Vaso-Occlusive Crises): Severe episodes of pain resulting from sickle-shaped cells obstructing blood flow.
- Acute Chest Syndrome: A life-threatening lung condition characterized by chest pain, fever, and difficulty breathing.
- Stroke: An increased risk stemming from blocked blood vessels in the brain, potentially causing long-term neurological damage.
- Organ Damage: Chronic damage affecting vital organs such as the kidneys, liver, and spleen.
- Increased Susceptibility to Infections: A compromised immune system makes individuals more vulnerable to infections.
- Anemia: Chronic fatigue and weakness due to a deficiency of healthy red blood cells.
Evolving Treatment Strategies for Sickle Cell Disease
Although a universal cure remains elusive, significant advancements in treatment are offering hope and improved quality of life for those with sickle cell disease.
Established and Emerging Therapies
- Hydroxyurea: A widely prescribed medication that reduces the frequency of pain crises by stimulating fetal hemoglobin production.
- Crizanlizumab (Adakveo): A newer medication approved for reducing the frequency of vaso-occlusive crises in adults and adolescents.
- Blood transfusions: A critical component of treatment, increasing the number of normal red blood cells and mitigating complications.
- Gene Therapy: Revolutionary treatments are becoming accessible through specialized programs, offering the potential for a functional cure.
- Bone Marrow Transplant: A potentially curative option, even though it carries significant risks and requires a matched donor.
Pro Tip: Maintaining adequate hydration, managing stress, and avoiding extreme temperatures can help minimize the risk of sickle cell crises.
The costs associated with managing sickle cell disease can be substantial. Numerous patient assistance programs and resources are available to help alleviate the financial burden. Organizations like the American Sickle Cell Anemia Association provide valuable guidance and support.
The Lifesaving Role of Blood Donations
Regular blood transfusions are frequently enough essential for individuals with sickle cell disease. Though, the demand for blood consistently outpaces the supply. Donations from diverse ethnic backgrounds are particularly crucial, as individuals with SCD benefit most from receiving blood that closely matches their genetic makeup. Less than 10% of Americans donate blood, highlighting the need for increased participation.
Early Detection: The Key to Effective Management
Prompt diagnosis is paramount for optimal management of sickle cell disease. Screening typically occurs:
- During routine newborn screening programs (within 24-48 hours of birth).
- As a standard component of prenatal care to determine carrier status.
- Through simple blood tests for adults who have not been previously screened.
Living Fully with Sickle Cell disease
Despite the challenges, individuals with sickle cell disease can lead fulfilling and productive lives with appropriate medical care, robust support systems, and access to essential resources. ongoing research continues to pave the way for innovative treatments and,ultimately,a cure.
What steps can be taken to foster greater understanding of sickle cell disease within our communities? What further research breakthroughs are needed to improve the lives of those affected?
Understanding Sickle Cell Disease Over Time
Research into sickle cell disease continues to evolve rapidly. Recent advancements in genomic medicine and gene editing offer promising avenues for developing more targeted and effective therapies. staying informed about these developments is vital for patients, families, and healthcare professionals alike.
Frequently Asked Questions About Sickle Cell Disease
- What is sickle cell disease? Sickle cell disease is a group of inherited red blood cell disorders that cause normally round red blood cells to become crescent-shaped, leading to blockages and health complications.
- How is sickle cell disease inherited? It’s inherited when a child receives a sickle cell gene from both parents. If only one parent carries the trait, the child is a carrier but usually doesn’t have the disease.
- What are the common symptoms of sickle cell disease? Common symptoms include pain crises, fatigue, anemia, frequent infections, and delayed growth.
- Is there a cure for sickle cell disease? While there isn’t a universal cure, bone marrow transplants and emerging gene therapies offer potential for a cure in some cases.
- How can I support research for sickle cell disease? you can donate to organizations dedicated to sickle cell research and raise awareness about the condition.
- Are there financial assistance programs available for sickle cell disease treatment? Yes, several patient assistance programs and resources can definitely help cover the costs of medication and treatment.
- What is the difference between sickle cell trait and sickle cell disease? Sickle cell trait means you carry one copy of the sickle cell gene, while sickle cell disease means you have two copies. Trait carriers usually don’t have symptoms.
Share this article and help raise awareness! Leave a comment below with yoru thoughts and experiences.
Breaking: Accessing Adakveo for Sickle Cell Disease: Cost savings and Assistance Programs Unveiled
Table of Contents
- 1. Breaking: Accessing Adakveo for Sickle Cell Disease: Cost savings and Assistance Programs Unveiled
- 2. Understanding Adakveo
- 3. Why is Adakveo So Costly?
- 4. Available Cost-Saving Programs
- 5. Novartis Oncology Universal Co-Pay Program
- 6. novartis Patient Assistance Foundation (NPAF)
- 7. Navigating Adakveo Costs: Key Takeaways
- 8. Final Thoughts
- 9. Evergreen Insights on Managing Medication Costs
- 10. Frequently Asked Questions About Adakveo Cost Assistance
- 11. how can I create a budget that aligns with my financial goals and lifestyle?
- 12. Essential data You Need: your Go-To Guide
- 13. Health & Wellness: Vital Data for a Healthy Life
- 14. Key Health Metrics You Must Know
- 15. Financial literacy: Mastering Your Finances
- 16. Essential Financial Concepts
- 17. creating A Budget: Step-by-step
- 18. Legal and Civic Knowledge: Understanding Your Rights and Responsibilities
- 19. Understanding Your Rights
- 20. Technology and Digital Literacy: staying Safe Online
- 21. Cyber Security Essentials
New york, June 19, 2025 – for individuals battling sickle cell disease, Adakveo, a vital treatment, can present significant financial challenges. Accessing this specialty medication is often intricate by insurance hurdles and substantial out-of-pocket expenses. Though, resources are available to ease this burden.
NeedyMeds, a non-profit organization, connects patients with programs designed to reduce medication costs, including Adakveo, irrespective of insurance status.This guide highlights manufacturer savings programs and other avenues for lowering Adakveo costs.
Understanding Adakveo
Adakveo (crizanlizumab-tmca) is a prescription infusion treatment aimed at minimizing vaso-occlusive crises (VOCs) in sickle cell disease (SCD) patients aged 16 and older. These VOCs, characterized by severe pain and complications, arise when sickled red blood cells obstruct blood flow.
The medication functions by targeting P-selectin, a molecule crucial in blood cell clumping. By inhibiting this molecule, Adakveo mitigates cell adhesion and inflammation, thereby reducing VOCs.
Typically, Adakveo is administered monthly following two initial loading doses. As a biologic infusion for a rare condition,its high cost necessitates cost-saving programs for many.
Why is Adakveo So Costly?
Adakveo’s high price stems from its nature as a biologic medication,produced using living cells through a complex manufacturing process.
Currently, no biosimilars for Adakveo are approved.However, Novartis, the drug’s manufacturer, provides programs to alleviate out-of-pocket expenses for eligible patients.
Available Cost-Saving Programs
Several programs can help reduce the financial strain of Adakveo treatment.
Novartis Oncology Universal Co-Pay Program
Patients with private or commercial insurance might potentially be eligible for Novartis’s Co-pay Program. Qualified individuals could pay as little as $25 per prescription, with annual coverage up to $15,000.
To qualify, patients must have private or commercial insurance that covers Adakveo. Upon activation, the co-pay card must be presented alongside the insurance card and prescription at a participating pharmacy. Reimbursement from other sources,like Flexible Spending accounts (FSAs),is not permitted.
Once the $15,000 annual limit is reached, patients are responsible for remaining costs.
Pro Tip: Always check the official program website for the most current terms and conditions.
novartis Patient Assistance Foundation (NPAF)
Uninsured, underinsured, or those denied coverage may receive free medication through the Novartis Patient Assistance Foundation. This program aids patients unable to afford treatment through insurance alone.
How the NPAF Works:
- applicants must submit a completed application with proof of income and U.S. residency.
- A healthcare provider must complete a separate form confirming the medical necessity of adakveo.
- Approved patients receive the medication at no cost for a specific duration, with the option to reapply for ongoing treatment.
For detailed application information, visit the NPAF program page.
Here is a summary of the programs available to help offset the cost of Adakveo:
| Program | Eligibility | Benefits |
|---|---|---|
| Novartis Oncology Universal Co-pay Program | Private or commercial insurance covering Adakveo | $25 per prescription,up to $15,000 per year |
| Novartis Patient Assistance Foundation (NPAF) | Uninsured,underinsured,or denied coverage | Free Adakveo medication for a set period |
Did You Know? Patient assistance programs often have income limitations. Check the specific requirements for each program.
Final Thoughts
Adakveo substantially improves the lives of individuals with sickle cell disease, but its cost can be a major obstacle. Manufacturer programs are available to reduce or eliminate out-of-pocket expenses, whether you have insurance or not.
For assistance in determining program eligibility, resources like NeedyMeds offer free tools, program listings, and personalized guidance via their Helpline at 800-503-6897.
Evergreen Insights on Managing Medication Costs
beyond specific programs for Adakveo, here are some evergreen strategies for managing prescription medication costs:
- Compare Prices: Pharmacies can have different prices for the same medication. Call around or use online tools to compare.
- Generic Alternatives: If available, ask your doctor about generic alternatives to branded medications.
- Review Insurance Coverage: Understand your insurance plan’s formulary and coverage rules.
- Tax Deductions: In the U.S., you may be able to deduct medical expenses exceeding 7.5% of your adjusted gross income.
Frequently Asked Questions About Adakveo Cost Assistance
how can I create a budget that aligns with my financial goals and lifestyle?
Essential data You Need: your Go-To Guide
Navigating the complexities of modern life requires access to essential information. Knowing where to find this crucial data and how to interpret it can considerably impact your decision-making and overall well-being. This guide provides a complete overview of the vital information you need, categorized for easy access.
Health & Wellness: Vital Data for a Healthy Life
Understanding your health is paramount. Accessing essential health information empowers you to make informed choices and maintain a healthy lifestyle. From preventive care to understanding symptoms, the right knowledge is key to taking care of yourself.
Key Health Metrics You Must Know
- Body mass Index (BMI): A measure of body fat based on height and weight.
- Blood Pressure: monitors the force of your blood against your artery walls.
- Cholesterol levels: Understanding your LDL, HDL, and total cholesterol is critical for heart health.
Regular check-ups and understanding these key health metrics are vital.Consulting a healthcare professional ensures you receive personalized guidance and care.
Financial literacy: Mastering Your Finances
Financial literacy is essential for achieving financial stability and reaching your financial goals. Accessing essential financial information and understanding financial concepts is key to success
Essential Financial Concepts
- Income vs. Expenses: Tracking the money coming in versus the money going out.
- Budgeting: Planning your spending to meet your financial goals.
- Investing: Using your money to generate wealth over time.
- Understanding Credit Scores: Understanding how your credit score influences lending terms.
creating A Budget: Step-by-step
Hear’s a simple budget framework you can start with:
| Category | Description | Allocated Budget |
|---|---|---|
| Housing | Rent/Mortgage, Utilities | 25-35% of Income |
| Transportation | Car Payments, Public Transit, Fuel | 10-15% of Income |
| Food | Groceries, Dining out | 10-15% of Income |
| Debt Payments | Credit Cards, Loans | As Needed, but ideally aiming to reduce debt |
| savings & Investing | Emergency Fund, Retirement, Investments | 10-20% of Income (or as much as possible) |
Legal and Civic Knowledge: Understanding Your Rights and Responsibilities
Knowing essential legal information and staying informed about your civic duties are crucial for becoming a responsible and engaged citizen.
Understanding Your Rights
- Constitutional Rights: Freedom of speech, religion, etc.
- Consumer Rights: Protection from unfair business practices
- Employment Rights: Fair labor standards and protections
Technology and Digital Literacy: staying Safe Online
In today’s digital age, essential tech information and digital literacy are paramount.
Cyber Security Essentials
- Strong Passwords: use complex and unique passwords.
- Scam Awareness: Recognizing phishing scams and fraudulent emails.
- Software Updates: Keeping your software updated to patch security vulnerabilities.
Pro Tip: Always back up your data regularly. Consider using cloud storage or external hard drives to keep your information safe.