Amazonian Harmony & Volcanic Fury: A Week in Global Science & Nature – Urgent Breaking News
This week’s visual dispatch from the front lines of science and nature is a powerful reminder of both the breathtaking beauty and the urgent fragility of our planet. From the delicate balance of life in the Amazon rainforest to the fiery displays of Hawaiian volcanoes, and the ongoing quest to understand our origins, these stories demand our attention. This is a breaking news update, optimized for Google News and SEO, bringing you the most compelling images and insights from around the globe.
Capybaras & Caimans: An Unexpected Amazonian Coexistence
The Amazon rainforest, often called the “lungs of the world,” continues to reveal its secrets. Photographers Gotzon Mantuliz and Rafa Fernandez Caballero recently captured stunning images showcasing the surprisingly peaceful coexistence of capybaras and caimans in the Amazonian floodplain. This isn’t simply a picturesque scene; it’s a testament to the complex ecological relationships that define this vital ecosystem. The Amazon is facing unprecedented threats from deforestation and climate change, making documentation of its biodiversity more critical than ever. Understanding these interactions is key to effective conservation efforts. Did you know the Amazon generates approximately 20% of the world’s oxygen? Protecting it isn’t just about saving trees; it’s about safeguarding the planet’s life support system.
A Silent Threat: Turtles Entangled in Ghost Nets
Photography isn’t always about celebrating beauty; sometimes, it’s about exposing harsh realities. A poignant image captured in the Balearic Sea by Sebnem Coskun / MARE depicts a sea turtle ensnared in a discarded fishing net – a chilling example of “bycatch.” Hundreds of marine animals die each year due to these “ghost nets,” which continue to trap wildlife long after being abandoned. The MARE awards recognized this image for its powerful message, highlighting the urgent need for sustainable fishing practices and responsible waste management. The problem of ghost nets is global, impacting marine ecosystems worldwide. Organizations like the Global Ghost Gear Initiative are working to mitigate this threat through removal programs and preventative measures.
Tinakula: A Volcanic Jewel Protecting Coral Biodiversity
Deep in the remote Solomon Islands lies Tinakula, a conical stratovolcano guarding some of the most biodiverse coral reefs on Earth. This unique site is part of the Coral Triangle, a region spanning six countries and containing 76% of the world’s coral species. The Solomon Islands recently pledged to preserve 24 million hectares of its marine waters, a crucial step in protecting this vital aquatic region. Coral reefs are often called the “rainforests of the sea,” providing habitat for a quarter of all marine life. However, they are incredibly vulnerable to climate change, pollution, and destructive fishing practices. The preservation of Tinakula and the Coral Triangle is paramount to maintaining global marine biodiversity.
Hawaii’s Kilauea: A Reminder of Earth’s Power
Volcanoes serve as a constant reminder of the dynamic geological forces shaping our planet. Kilauea volcano in Hawaii has been particularly active recently, with tongues of fire exceeding 100 meters in height. Over the past 12 months, 37 eruptive episodes have been recorded. While volcanic eruptions can be destructive, they also play a vital role in creating new land and enriching soil. Understanding volcanic activity is crucial for hazard mitigation and ensuring the safety of communities living near these powerful natural phenomena. The Hawaiian Volcano Observatory provides real-time monitoring and research on Kilauea and other Hawaiian volcanoes.
The Mighty Mantis Shrimp: A Tiny Powerhouse
Don’t let its size fool you. The mantis shrimp (Gonodactylus smithii), though rarely exceeding eight centimeters, is a formidable predator. Its limbs can break glass and it can move at speeds of up to 80 kilometers per hour. This incredible creature showcases the remarkable adaptations found throughout the natural world. Mantis shrimp possess some of the most complex visual systems known to science, with the ability to see polarized light and a wider range of colors than humans. Their powerful strikes are used to smash open shells and capture prey.
Atapuerca: Rewriting Human History
Just a few kilometers from Burgos, Spain, the archaeological site of Atapuerca is yielding groundbreaking discoveries about human evolution. Four decades of excavations have revealed remains from five different species of hominids, rewriting our understanding of our ancestors. The findings at Atapuerca provide crucial insights into the migration patterns and evolutionary relationships of early humans. This site is a UNESCO World Heritage site and continues to be a focus of intense scientific research.
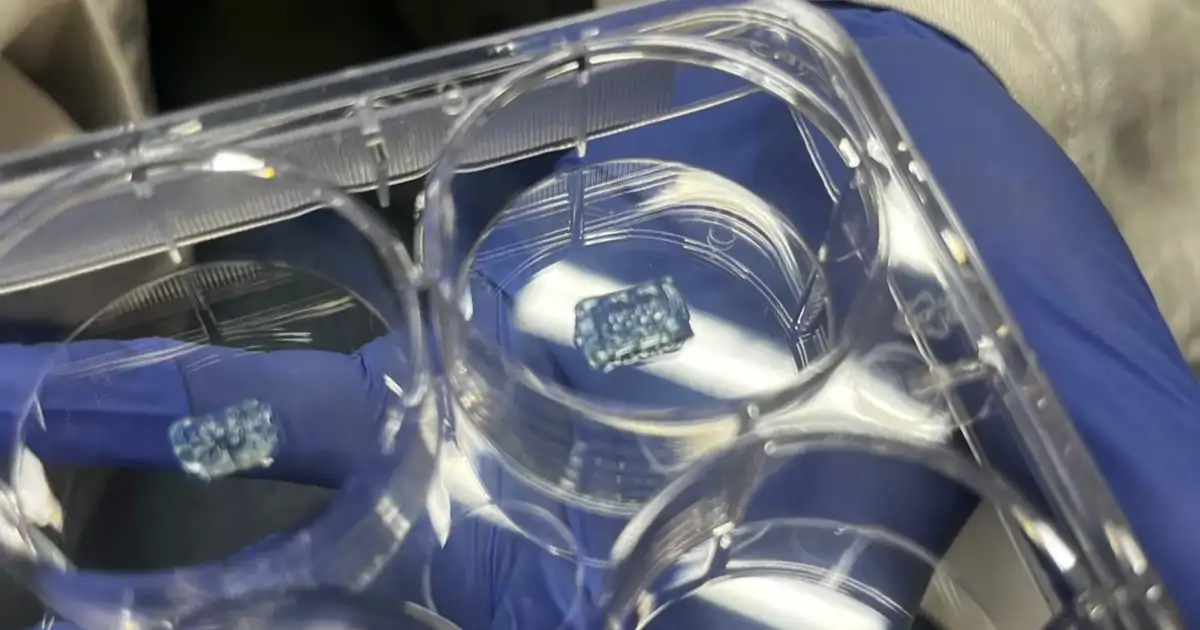
Artemis II: Preparing for a Lunar Return
The four astronauts of the Artemis II mission are nearing the completion of their 18-month training program, preparing for a historic return to the Moon. Their training includes a surprising exercise: simulated spacewalks in a giant pool. This allows them to experience the weightlessness of space and practice essential tasks in a controlled environment. The Artemis program represents a new era of lunar exploration, with the goal of establishing a sustainable human presence on the Moon and eventually using it as a stepping stone for missions to Mars. This mission is a testament to human ingenuity and our enduring desire to explore the cosmos.
These stories, captured in stunning imagery and backed by scientific rigor, underscore the interconnectedness of our planet and the importance of continued exploration and conservation. Stay tuned to archyde.com for more breaking news and in-depth coverage of the world around us. Explore our archives for further insights into these topics and discover the latest developments in science, nature, and technology.