Nipah Virus: Beyond the Outbreak – Forecasting Future Risks and Preparedness
A chilling reminder of nature’s potential for disruption arrived at the close of 2023: five confirmed cases of Nipah virus in West Bengal, India. With a mortality rate that can climb as high as 75%, depending on healthcare capacity, this zoonotic disease isn’t just a regional health concern – it’s a harbinger of escalating risks in a world grappling with climate change, deforestation, and increasing human-animal interaction. But what does this outbreak tell us about the future of Nipah, and how can we prepare for a potential surge in zoonotic threats?
The Expanding Threat Landscape: Why Nipah Matters Now More Than Ever
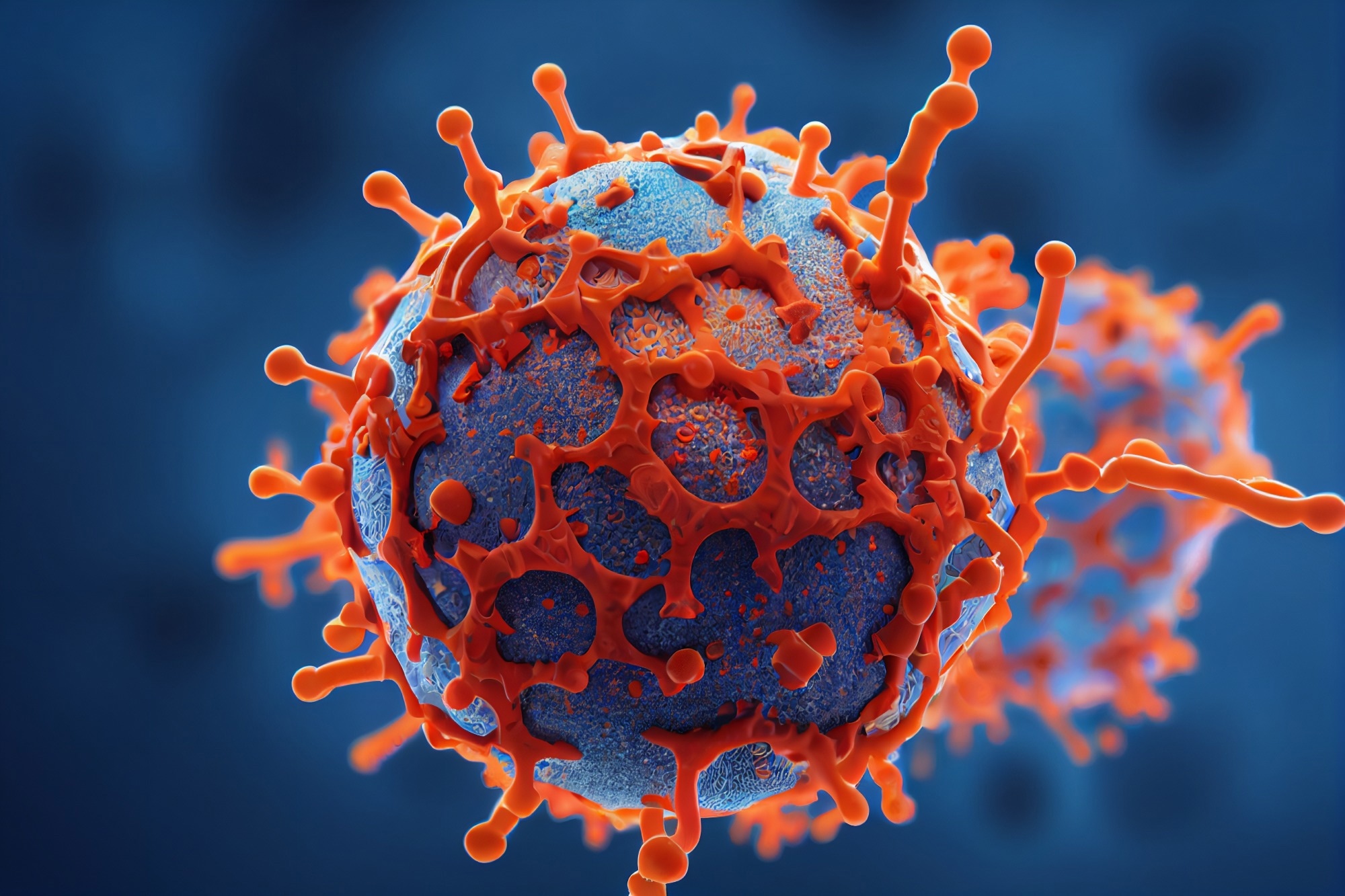
Nipah virus (NiV) isn’t new. First identified in Malaysia in 1999, it’s resurfaced repeatedly in South and Southeast Asia, primarily Bangladesh and India. Transmitted from fruit bats to humans (and sometimes person-to-person), NiV causes a range of symptoms, from mild respiratory illness to fatal encephalitis. The recent outbreak, affecting healthcare workers alongside others, underscores the virus’s ability to rapidly spread within communities and strain already burdened healthcare systems. However, the increasing frequency and geographic spread of outbreaks aren’t random. They’re a direct consequence of environmental changes that are bringing humans into closer contact with bat populations.
Did you know? Over 80% of emerging infectious diseases originate in animals, highlighting the critical link between environmental health and human health.
Climate Change, Deforestation, and the Bat Factor
Deforestation, driven by agricultural expansion and urbanization, is forcing bats to seek new habitats – often in closer proximity to human settlements. Simultaneously, climate change is altering bat migration patterns and fruiting seasons, further disrupting their natural behaviors and increasing the likelihood of spillover events. A recent study published in Nature Climate Change suggests that the geographic range suitable for NiV-carrying bats could expand significantly in the coming decades, potentially exposing millions more people to the virus. This isn’t simply about Nipah; it’s a pattern we’re seeing with other zoonotic diseases like Ebola and SARS-CoV-2.
Beyond Bats: Understanding the Transmission Pathways
While bats are the primary reservoir, NiV transmission isn’t limited to direct contact. Contaminated food, particularly date palm sap in Bangladesh, is a significant pathway. Person-to-person transmission, though requiring close contact with bodily fluids, is also a major concern, as evidenced by the infections among healthcare workers in West Bengal. This highlights the critical need for robust infection control protocols and rapid response teams equipped to contain outbreaks.
The Role of Livestock as Amplifiers
In the 1999 Malaysian outbreak, pigs acted as an intermediate host, amplifying the virus and accelerating its spread. While this hasn’t been a consistent pattern in subsequent outbreaks, the potential for livestock to play a similar role remains a significant concern. Monitoring livestock populations in areas with high bat activity is crucial for early detection and prevention.
Future Trends: What to Expect in the Next Decade
Several key trends will shape the future of Nipah and other zoonotic disease threats:
- Increased Surveillance: We’ll see a growing emphasis on proactive surveillance, not just in known hotspots but also in areas where environmental changes are increasing risk. This will involve monitoring bat populations, livestock, and human populations for early signs of infection.
- Advanced Diagnostics: Rapid and accurate diagnostic tools are essential for containing outbreaks. Expect advancements in point-of-care diagnostics, allowing for faster identification of cases in resource-limited settings.
- Vaccine Development: While a fully effective Nipah vaccine remains elusive, significant progress is being made. Several vaccine candidates are in preclinical and clinical trials, offering hope for a preventative measure in the future.
- One Health Approach: The recognition that human, animal, and environmental health are interconnected will drive a more integrated “One Health” approach to disease prevention and control.
- AI-Powered Prediction: Artificial intelligence and machine learning will play an increasingly important role in predicting outbreaks by analyzing environmental data, animal movement patterns, and human behavior.
Expert Insight: “The Nipah virus outbreak in West Bengal serves as a stark reminder that we are living in an age of increasing zoonotic risk. Investing in proactive surveillance, research, and preparedness is not just a public health imperative – it’s an economic necessity.” – Dr. Anya Sharma, Epidemiologist, Global Health Institute.
Preparing for the Inevitable: Actionable Steps for Individuals and Communities
While the threat of Nipah and other zoonotic diseases is real, it’s not insurmountable. Here are some actionable steps individuals and communities can take:
- Practice Good Hygiene: Frequent handwashing, especially after contact with animals or potentially contaminated surfaces, is crucial.
- Avoid Contact with Bats: Do not handle bats or their droppings. If you encounter a sick or dead bat, contact local authorities.
- Consume Safe Food: Avoid consuming raw date palm sap or other potentially contaminated food products.
- Support Sustainable Land Use: Advocate for policies that promote sustainable land use practices and protect natural habitats.
- Stay Informed: Keep up-to-date on the latest information about zoonotic diseases from reputable sources like the WHO and CDC.
Pro Tip: If you live in an area with a high risk of Nipah virus, familiarize yourself with the symptoms and seek medical attention immediately if you experience fever, headache, or other concerning symptoms.
Frequently Asked Questions
What is the treatment for Nipah virus?
Currently, there is no specific antiviral treatment for Nipah virus infection. Treatment is primarily supportive, focusing on managing symptoms and preventing complications. Intensive care is often required.
How contagious is Nipah virus?
Nipah virus is not as easily transmitted as some other viruses, like influenza. However, it can spread through close contact with infected individuals, their bodily fluids, or contaminated materials. Person-to-person transmission is a significant concern in outbreak settings.
Can Nipah virus cause long-term health problems?
Yes. Even after recovering from acute Nipah virus infection, some individuals may experience long-term neurological sequelae, such as seizures, personality changes, or cognitive impairment. Late relapses have also been reported.
What is being done to prevent future Nipah outbreaks?
Efforts to prevent future outbreaks include surveillance of bat populations, monitoring livestock, improving hygiene practices, developing vaccines, and promoting a One Health approach to disease prevention and control.
The Nipah virus outbreak in West Bengal is a wake-up call. It’s a reminder that the threat of zoonotic diseases is growing, and that we must invest in preparedness, research, and sustainable practices to protect ourselves and future generations. The future of global health depends on our ability to anticipate, prevent, and respond effectively to these emerging threats. What steps will you take to stay informed and prepared?