RSV Vaccination: Beyond the Current Strategy – Predicting the Next Wave of Prevention
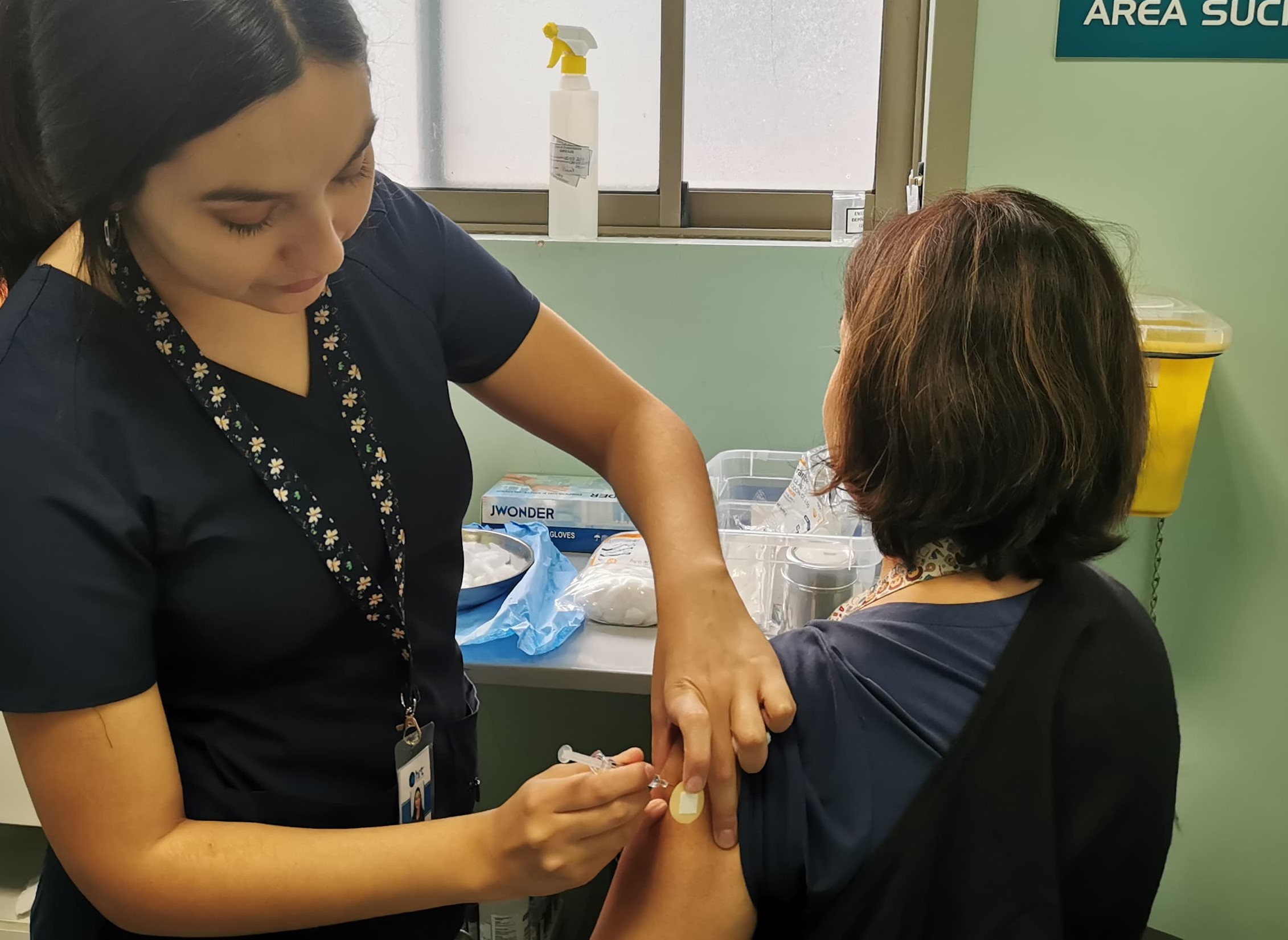
Imagine a future where a routine fall vaccination protects not just against flu and COVID-19, but also against a potentially debilitating respiratory illness often dismissed as ‘just a cold.’ That future is rapidly approaching with the advent of RSV vaccines, but the story doesn’t end with the current recommendations. While initial vaccination strategies focus on high-risk adults, the evolving understanding of RSV’s impact suggests a broader, more dynamic approach is on the horizon.
The Expanding Landscape of RSV Risk
Currently, RSV vaccination guidelines prioritize individuals 60 and older, those with specific immunocompromising conditions, and pregnant people to protect newborns. However, emerging research hints at a wider spectrum of vulnerability. Recent studies are exploring the impact of RSV on individuals with stable chronic conditions – like diabetes or kidney disease – who may not currently qualify for vaccination but experience significant health burdens from RSV infection. This raises a critical question: will the definition of “high risk” expand, and if so, how quickly?
The initial rollout of RSV vaccines has already demonstrated a positive impact, with a slight reduction in disease burden observed during the 2024-2025 season in Spain, as reported by health authorities. However, maintaining this momentum requires proactive adaptation. A key takeaway is that a static vaccination strategy will quickly become outdated.
The Role of Real-World Data and Post-Market Surveillance
The recent authorization of RSV vaccines is a landmark achievement, but it’s also the beginning of a crucial data-gathering phase. Long-term efficacy, duration of protection, and the potential need for booster doses remain open questions. Robust post-market surveillance, coupled with real-world data analysis, will be paramount in refining vaccination recommendations. We can expect to see a more nuanced understanding of vaccine effectiveness across different age groups, comorbidities, and even geographic regions.
RSV vaccination isn’t a ‘one-size-fits-all’ solution. Personalized approaches, informed by individual risk profiles and immune responses, may become increasingly common.
Beyond Vaccination: Integrated Prevention Strategies
While vaccination is the cornerstone of RSV prevention, a holistic approach will likely emerge. This includes strengthening infection control measures in healthcare settings, promoting respiratory hygiene (handwashing, masking during outbreaks), and exploring novel preventative therapies. The lessons learned from the COVID-19 pandemic – particularly the importance of layered interventions – will undoubtedly inform future RSV prevention strategies.
One area of growing interest is the potential for maternal vaccination to provide extended protection to infants, even beyond the initial months of life. Further research is needed to determine the optimal timing and dosage of maternal RSV vaccination to maximize infant protection. This could significantly reduce the burden of RSV-related hospitalizations in young children.
The Convergence of RSV and Other Respiratory Viruses
RSV rarely operates in isolation. Coinfection with influenza, SARS-CoV-2, and other respiratory viruses is common, often leading to more severe illness. This highlights the need for integrated diagnostic testing and coordinated prevention efforts. Imagine a future where a single nasal swab can simultaneously detect multiple respiratory pathogens, allowing for targeted antiviral treatment and informed public health interventions. The CDC provides comprehensive information on RSV and its impact.
The Technological Frontier: Rapid Diagnostics and Personalized Vaccines
The development of rapid, point-of-care RSV diagnostics is crucial for timely diagnosis and treatment. Currently, RSV testing often requires laboratory analysis, which can delay results. Faster, more accessible diagnostic tools will empower healthcare providers to make informed decisions and initiate appropriate interventions more quickly.
Looking further ahead, the potential for personalized RSV vaccines – tailored to an individual’s immune profile and risk factors – is an exciting prospect. Advances in mRNA technology, which proved pivotal in the development of COVID-19 vaccines, could pave the way for customized RSV vaccines that offer enhanced protection. This is still several years away, but the groundwork is being laid now.
Frequently Asked Questions
What are the current recommendations for RSV vaccination?
Currently, RSV vaccines are recommended for adults 60 years and older, individuals with certain immunocompromising conditions, and pregnant people during the third trimester of pregnancy.
How effective are the current RSV vaccines?
Clinical trials have demonstrated that RSV vaccines are highly effective in preventing severe RSV-related illness, hospitalization, and mortality in the target populations. Real-world data is still being collected to assess long-term efficacy.
Will RSV vaccination become an annual recommendation?
The need for annual RSV vaccination is currently unknown. Ongoing research will determine the duration of protection provided by the vaccines and whether booster doses are necessary.
What can I do to protect myself from RSV if I don’t qualify for vaccination?
Practice good respiratory hygiene, including frequent handwashing, covering coughs and sneezes, and avoiding close contact with sick individuals. Consider wearing a mask in crowded indoor settings during peak RSV season.
The future of RSV prevention is dynamic and multifaceted. While the current vaccines represent a significant step forward, continuous innovation, data-driven decision-making, and a holistic approach to respiratory health will be essential to minimize the burden of this often-underestimated virus. What are your predictions for the evolution of RSV prevention? Share your thoughts in the comments below!