Chikungunya’s Global Resurgence: Predicting the Next Wave of Outbreaks
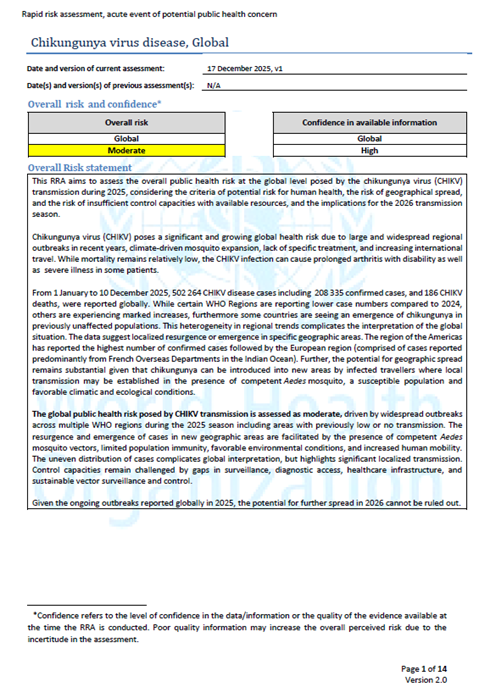
Imagine a future where a mosquito bite isn’t just an itchy nuisance, but a potential gateway to debilitating joint pain lasting months, even years. This isn’t science fiction; it’s a growing reality as the chikungunya virus expands its reach, fueled by climate change and increasing global travel. A recent WHO Rapid Risk Assessment highlights the escalating threat, but what does this mean for the future of public health, and how can we prepare for a potential surge in cases?
Understanding the Expanding Threat Landscape
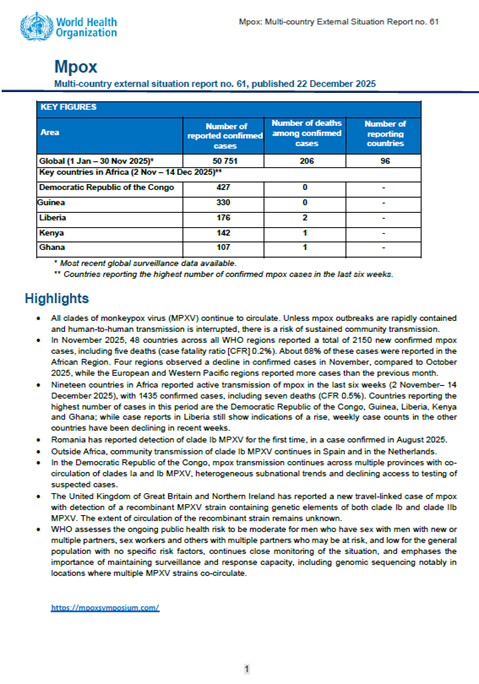
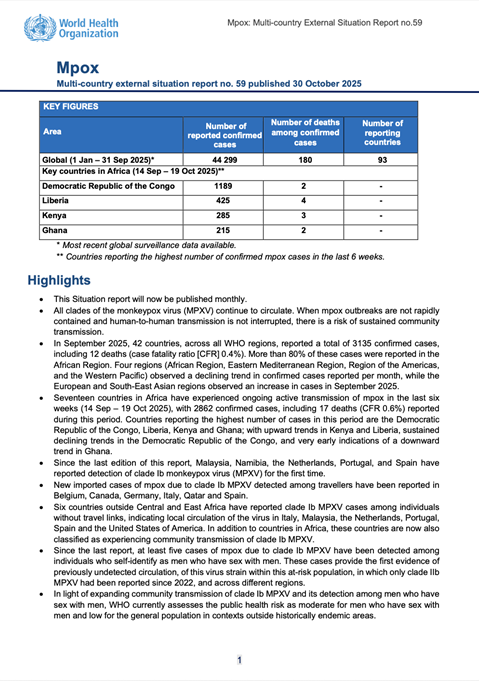
The WHO’s recent assessment underscores a critical point: **chikungunya virus** is no longer confined to traditionally endemic regions. While historically concentrated in Africa, Asia, and the Indian Ocean islands, the virus is now establishing itself in new territories, including the Americas and parts of Europe. This geographical spread is driven by several interconnected factors. The primary vector, Aedes aegypti and Aedes albopictus mosquitoes, are highly adaptable and thrive in urban environments, making them efficient transmitters in densely populated areas. Furthermore, increased international travel facilitates the movement of infected individuals, introducing the virus to previously unaffected regions.
The public health impact is significant. Chikungunya causes fever and severe joint pain, often debilitating enough to prevent daily activities. While fatalities are rare, the chronic arthralgia (joint pain) can persist for months or years, significantly impacting quality of life. The economic burden associated with healthcare costs and lost productivity is also substantial.
Climate Change: A Key Accelerator
Climate change is arguably the most significant driver of this expansion. Rising temperatures and altered rainfall patterns are expanding the geographical range of Aedes mosquitoes, creating suitable breeding grounds in areas previously inhospitable. Warmer temperatures also accelerate the virus’s replication rate within the mosquito, increasing transmission efficiency. According to recent studies, the potential range of both Aedes aegypti and Aedes albopictus is projected to increase significantly in the coming decades, putting billions more people at risk.
Pro Tip: Simple measures like eliminating standing water around your home – in flower pots, tires, and gutters – can significantly reduce mosquito breeding sites and your risk of infection.
Predicting Future Trends: Beyond Geographical Spread
The future of chikungunya isn’t just about where the virus will spread; it’s about how it will spread and evolve. Several key trends are emerging:
- Emergence of New Viral Strains: The virus is constantly evolving. New strains with potentially increased virulence or altered transmission dynamics could emerge, posing a challenge to existing diagnostic tools and vaccine development efforts.
- Co-infection Risks: The possibility of co-infection with other mosquito-borne viruses, such as dengue and Zika, is a growing concern. Co-infection can lead to more severe disease outcomes and complicate diagnosis.
- Urbanization and Population Density: Continued urbanization and increasing population density in vulnerable regions will exacerbate transmission rates, creating ideal conditions for outbreaks.
- Strain Variation and Immunity: Prior exposure to one strain of chikungunya doesn’t necessarily provide complete protection against others. This means populations previously affected by the virus may remain susceptible to new outbreaks caused by different strains.
“Did you know?” Chikungunya’s name comes from the Makonde language, spoken in Tanzania and Mozambique, and means “that which bends up,” referring to the contorted posture sufferers adopt due to joint pain.
Insufficient Control Capacities: A Global Weakness
The WHO assessment also highlights a critical vulnerability: insufficient control capacities in many affected countries. Limited access to diagnostic tools, inadequate surveillance systems, and a lack of trained healthcare personnel hinder effective outbreak response. Resource constraints often prevent the implementation of comprehensive vector control programs, such as mosquito spraying and larval source management. This is particularly concerning in low- and middle-income countries, where the burden of disease is highest.
Expert Insight: “Effective chikungunya control requires a multi-faceted approach, combining vector control, surveillance, clinical management, and community engagement. Investing in these areas is crucial to mitigating the risk of future outbreaks.” – Dr. Anya Sharma, Global Health Epidemiologist.
Actionable Insights: Preparing for the Future
While the threat of chikungunya is real, proactive measures can significantly reduce the risk. Here are some key strategies:
- Strengthen Surveillance Systems: Investing in robust surveillance systems is essential for early detection and rapid response to outbreaks. This includes improved laboratory capacity, real-time data collection, and effective reporting mechanisms.
- Enhance Vector Control: Implementing comprehensive vector control programs, including mosquito spraying, larval source management, and community education, is crucial for reducing mosquito populations.
- Develop and Deploy Vaccines: While a chikungunya vaccine is currently available, wider access and affordability are critical. Continued research and development efforts are needed to improve vaccine efficacy and address emerging viral strains.
- Improve Clinical Management: Training healthcare personnel to accurately diagnose and manage chikungunya cases is essential for providing appropriate care and reducing the burden of chronic arthralgia.
- Promote Public Awareness: Educating the public about the virus, its transmission, and preventive measures is crucial for empowering individuals to protect themselves.
See our guide on Mosquito-Borne Illness Prevention for more detailed information on protecting yourself and your family.
Frequently Asked Questions
Q: What are the symptoms of chikungunya?
A: Common symptoms include fever, severe joint pain (especially in the hands and feet), headache, muscle pain, and rash.
Q: Is there a cure for chikungunya?
A: There is no specific cure for chikungunya. Treatment focuses on relieving symptoms, such as pain and fever.
Q: How can I protect myself from chikungunya?
A: Use mosquito repellent, wear long sleeves and pants, eliminate standing water around your home, and use mosquito nets.
Q: Can chikungunya be fatal?
A: Fatalities are rare, but the chronic joint pain can significantly impact quality of life.
The resurgence of chikungunya demands a global, coordinated response. By investing in research, strengthening public health infrastructure, and empowering communities, we can mitigate the risk and protect vulnerable populations from this debilitating disease. The future isn’t predetermined; it’s shaped by the actions we take today.
What are your predictions for the future of mosquito-borne diseases? Share your thoughts in the comments below!