Breaking: New Data Reveals Regional Disparities in Influenza Mortality
health. Stay informed!">
Influenza Mortality Trends exhibit significant regional differences, according to a new study. Researchers have identified key viral strains contributing to these disparities, with implications for public health strategies. Understanding these trends is crucial for effective prevention and treatment.
Regional Differences in Influenza-Associated Mortality
A recent analysis reveals notable differences in influenza mortality between northern and southern regions. The northern region experienced higher influenza-associated excess mortality for all causes and pneumonia & influenza (P&I) in 2015, with rates of 25.29 and 0.81 per 100,000 people, respectively, compared to 4.61 and 0.69 in the south. Conversely, the excess respiratory mortality (ERM) related to influenza was higher in the southern region at 5.34 per 100,000 persons versus 2.69 in the north.
These variations highlight the complex interplay of factors influencing influenza’s impact across different geographical areas.
Key Years and Mortality Peaks
Certain years showed marked increases in influenza-associated excess mortality. Specifically, 2014, and 2017-2019 recorded elevated rates across all categories. For example,in 2017,excess mortalities reached 40.69 per 100,000 for all causes, 1.71 for P&I, and 5.00 for respiratory diseases.
Did You Know? Analyzing mortality data can provide crucial insights into the effectiveness of vaccination campaigns and public health interventions.
Dominant Influenza Subtypes: A/H1N1 and Influenza B
The influenza A/H1N1 subtype emerged as a significant driver of excess mortality between 2012 and 2019. In the northern region, it accounted for 13.72 per 100,000 persons for all-cause mortality. Simultaneously occurring, Influenza B contributed more substantially to excess all-cause and respiratory mortality in the southern region compared to the north.
These patterns underscore the importance of monitoring specific viral strains to tailor public health responses.

Contribution of mortality from 2012 to 2021. the left column refers to the northern region (A, C, E), and the right column refers to the southern region (B, D, F).P&I pneumonia and influenza
Decline in Influenza A Mortality During Pandemic Years
Notably, a substantial decrease in excess mortality attributable to influenza A occurred between 2020 and 2021, coinciding with the COVID-19 pandemic. Specifically, influenza A/H1N1-related excess all-cause mortality fell from 2.62 to 0.31 per 100,000 in the northern region and from 3.79 to 0.24 in the southern region.
This decline might be attributed to public health measures implemented to combat COVID-19, which also reduced influenza transmission.
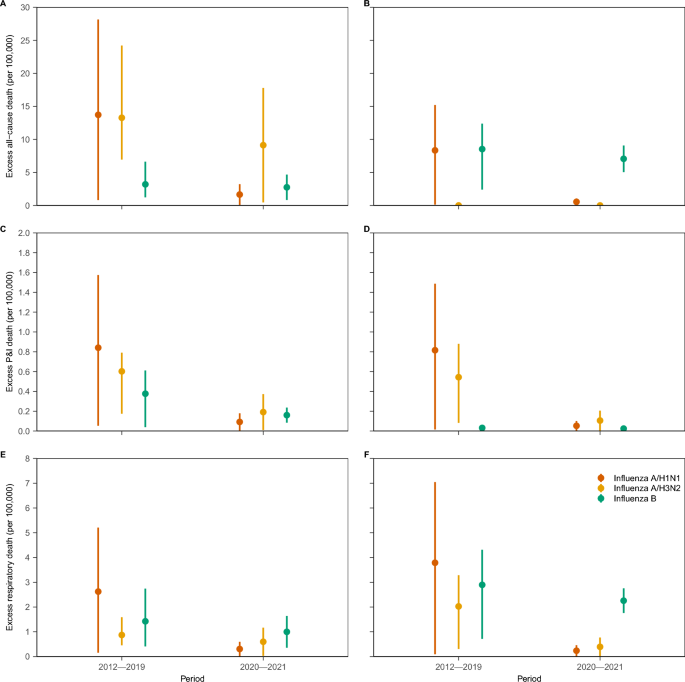
Influenza-associated mortality during 2012-2019 and 2020-2021 by influenza subtype.The left column refers to the northern region (A, C, E), and the right column refers to the southern region (B, D, F). P&I pneumonia and influenza
Impact of Meteorological Factors on Mortality
Lagged correlation analysis indicated that influenza virus activity, temperature, absolute humidity, and relative humidity were significantly correlated with mortality. Respiratory death showed a stronger correlation in both regions. Although most meteorological factors were negatively correlated with death, absolute humidity showed a relatively high correlation.
Evergreen Insights into Influenza Management
Understanding the dynamics of influenza mortality involves considering multiple factors beyond viral strains. Public health interventions, vaccination strategies, and environmental conditions all play critical roles. recent data from the Centers for Disease Control and Prevention (CDC) shows that annual flu vaccinations can reduce the risk of influenza illness by 40% to 60% when the vaccine strains closely match circulating viruses. This emphasizes the ongoing need for effective vaccine development and widespread immunization efforts.
Pro Tip: Staying informed about local influenza trends and understanding the impact of environmental factors can help individuals and communities take proactive steps to mitigate risks.
comparative Analysis of Influenza Seasons
To better understand the impact of influenza across different seasons, consider the following comparison:
| Year | All-Cause Mortality (per 100,000) | P&I Mortality (per 100,000) | Respiratory Mortality (per 100,000) |
|---|---|---|---|
| 2014 | 31.47 | 1.89 | 5.02 |
| 2017 | 40.69 | 1.71 | 5.00 |
| 2018 | 30.38 | 1.88 | 5.95 |
| 2019 | 49.23 | 2.86 | 8.68 |
This table illustrates the variability in influenza-associated mortality across different years, highlighting the need for continuous monitoring and adaptive public health strategies.
Frequently Asked Questions about Influenza Mortality
- What is influenza mortality? Influenza mortality refers to deaths directly or indirectly related to influenza infections.
- How is influenza mortality measured? It is often measured by assessing excess mortality rates during influenza seasons compared to baseline periods.
- why does influenza mortality vary by region? Regional variations can be attributed to differences in climate, population density, access to healthcare, and prevalent viral strains.
- What are the primary causes of influenza-related deaths? Pneumonia and other respiratory complications are major contributors to influenza mortality.
- How effective are flu vaccines in reducing mortality? Flu vaccines can significantly reduce the risk of severe illness and death, especially in high-risk groups.
- Can meteorological factors influence influenza mortality rates? Yes, temperature, humidity, and other weather conditions can impact the transmission and severity of influenza.
What measures do you think are most effective in reducing influenza mortality? Share your thoughts in the comments below.
Disclaimer: This article provides general information and should not be considered medical advice. Consult with a healthcare professional for personalized guidance and treatment.
