This text discusses a new measure called dunedinpacni that assesses biological aging based on brain imaging data. Here’s a breakdown of the key points:
What is DunedinPACNI?
It’s a publicly available measure developed by researchers.
It uses brain imaging data to determine how fast someone is aging biologically.
How was it tested and what were the findings?
The measure was applied to three large datasets: the Alzheimer’s Disease Neuroimaging Initiative (ADNI), UK Biobank, and BrainLat.
Faster DunedinPACNI scores predicted:
cognitive impairment.
Accelerated brain atrophy (shrinkage).
Conversion to mild cognitive impairment (MCI) or dementia.
Specific examples:
In ADNI,individuals in the top 10% for fast aging had a 61% higher risk of progressing to MCI or dementia. They also experienced memory problems earlier. In UK Biobank, faster DunedinPACNI predicted a 14% higher likelihood of being diagnosed with chronic age-related diseases.
Those aging fastest also faced an 18% higher risk of chronic diseases, worse cognitive performance, higher frailty, and poorer self-rated health. over 10 years, the fastest agers were 41% more likely to die.
Social gradients: DunedinPACNI reflects health inequities, with faster aging scores observed in individuals with less education or lower income.
Cross-cultural relevance: The measure also showed predictive power for dementia risk and cognitive impairment in Latin American adults (BrainLat cohort).Future Potential and Applications:
Current limitation: DunedinPACNI is currently a relative measure, comparing individuals within a given dataset. it doesn’t yet provide an absolute measure of how someone is aging compared to the general population.
Development of Norms: Researchers are working on developing normative reference charts, similar to those for height or BMI, which will allow for absolute comparisons. These are expected within a year.
Clinical practice: Once reference norms are established, DunedinPACNI coudl be adopted in clinical practice within a few years.
Research Applications:
Outcome measure in clinical trials: To assess the effectiveness of interventions aimed at slowing aging.
Biomarker for accelerated aging: To predict the likelihood of cognitive decline (normal to MCI, MCI to dementia).
Surrogate outcome for AD interventions: In younger individuals, it could show an intervention slows aging, a key dementia risk factor, even before dementia symptoms appear.
Screening tool in AD clinical trials: To select participants with similar aging rates or exclude those aging too rapidly to potentially avoid adverse effects.
In essence, DunedinPACNI is a promising new tool for understanding and measuring biological aging, with significant potential for both research and future clinical applications in the study and management of age-related diseases, particularly Alzheimer’s.
What is “brain age” and how does it differ from chronological age in the context of dementia risk?
Table of Contents
- 1. What is “brain age” and how does it differ from chronological age in the context of dementia risk?
- 2. Brain MRI predicts Aging and Dementia Risk with Single Scan
- 3. Understanding Brain Age and Cognitive Decline
- 4. How Does a brain MRI predict Dementia Risk?
- 5. The role of AI and Machine Learning in Predictive Modeling
- 6. Benefits of Early Dementia Risk Prediction
- 7. Practical Considerations and Limitations
- 8. Real-World Examples & Ongoing Research
Brain MRI predicts Aging and Dementia Risk with Single Scan
Understanding Brain Age and Cognitive Decline
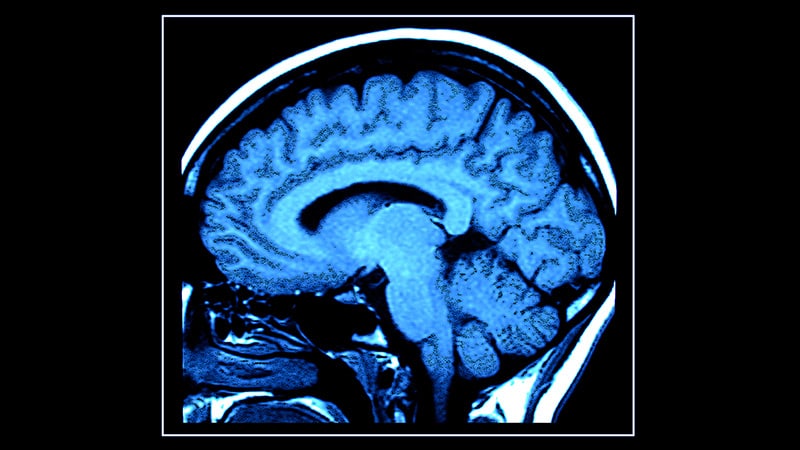
For years, assessing an individual’s risk for dementia involved lengthy cognitive tests and tracking symptoms over time. Now, advancements in neuroimaging, specifically brain MRI, are offering a revolutionary approach: predicting future cognitive decline and dementia risk with a single scan.This isn’t about determining chronological age, but rather measuring brain age, a metric derived from MRI scans that reflects the structural and functional health of the brain. A discrepancy between chronological age and brain age can be a significant indicator of accelerated aging and increased dementia vulnerability.
How Does a brain MRI predict Dementia Risk?
the process leverages refined image analysis techniques,frequently enough employing artificial intelligence (AI) and machine learning (ML) algorithms. These algorithms are trained on vast datasets of brain scans from individuals with and without dementia, identifying subtle patterns and biomarkers indicative of future cognitive impairment.
Here’s a breakdown of what the MRI assesses:
Gray Matter Volume: Loss of gray matter, notably in regions like the hippocampus (crucial for memory) and the prefrontal cortex (responsible for executive functions), is a hallmark of Alzheimer’s disease and other dementias.
White Matter Integrity: White matter tracts connect different brain regions. damage to these tracts, frequently enough visualized as “white matter lesions” on MRI, disrupts dialog and contributes to cognitive decline. Diffusion Tensor Imaging (DTI) is a specific MRI technique used to assess white matter integrity.
Amyloid and Tau Deposits: While not always visible on standard MRI,specialized MRI techniques like amyloid PET scans (frequently enough used in conjunction with structural MRI) can detect the buildup of amyloid plaques and tau tangles – proteins strongly associated with Alzheimer’s disease.
Brain Atrophy patterns: Specific patterns of brain shrinkage can indicate the type of dementia a person is highly likely to develop. For example, frontotemporal dementia often presents with atrophy in the frontal and temporal lobes.
Functional Connectivity: Functional MRI (fMRI) measures brain activity by detecting changes associated with blood flow. Altered functional connectivity patterns can precede noticeable cognitive symptoms.
The role of AI and Machine Learning in Predictive Modeling
The sheer volume of data generated by brain MRIs necessitates the use of AI and ML. These technologies can identify subtle changes that might be missed by the human eye, and build predictive models with remarkable accuracy.
Deep Learning: A subset of ML, deep learning algorithms are particularly effective at analyzing complex image data like brain MRIs.
Radiomics: this field extracts a large number of quantitative features from medical images (like MRIs) and uses them to build predictive models.
Predictive Biomarkers: AI helps identify the most reliable biomarkers – measurable indicators of a biological state or condition – for predicting dementia risk.
Benefits of Early Dementia Risk Prediction
Identifying individuals at high risk for dementia before symptoms appear offers several key advantages:
Proactive Lifestyle Changes: Individuals can adopt lifestyle modifications known to promote brain health, such as regular exercise, a healthy diet (like the MIND diet), cognitive stimulation, and social engagement.
Early Intervention: While there’s currently no cure for most dementias, early intervention with available medications and therapies can help manage symptoms and slow disease progression.
Clinical Trial Eligibility: Early identification allows individuals to participate in clinical trials testing new treatments and preventative strategies.
Financial and Legal Planning: Knowing one’s risk allows for proactive financial and legal planning, ensuring wishes are respected and care is arranged.
Reduced Anxiety: While a risk prediction isn’t a diagnosis, it can empower individuals to take control of their health and prepare for the future.
Practical Considerations and Limitations
While promising, brain MRI-based dementia risk prediction isn’t without its limitations:
Cost and Accessibility: MRIs are expensive and not universally accessible.
false Positives and False Negatives: Predictive models aren’t perfect. There’s a risk of incorrectly identifying individuals as high-risk (false positive) or failing to identify those who will develop dementia (false negative).
Ethical Considerations: The psychological impact of receiving a high-risk prediction needs careful consideration. Genetic counseling and support services are crucial.
Need for Longitudinal Studies: Continued research and long-term follow-up studies are essential to refine predictive models and validate their accuracy.
standardization of Protocols: Variations in MRI scanners and imaging protocols can affect the reliability of results. Standardization is crucial.
Real-World Examples & Ongoing Research
Several research initiatives are pushing the boundaries of dementia risk prediction using brain MRI:
The Alzheimer’s Disease Neuroimaging Initiative (ADNI): A landmark study that has generated a wealth of data on brain imaging,biomarkers,and cognitive function in individuals with and without Alzheimer’s disease.
Framingham Heart Study: This long-running study is now incorporating brain MRI data to investigate the relationship between cardiovascular health and brain aging.
* University of California, San Francisco (UCSF) Memory and Aging Centre: Researchers at UCSF are developing AI-powered tools to predict dementia risk based on brain MRI scans.
These studies are demonstrating that it’s increasingly possible to identify individuals at risk for dementia years, even decades, before symptoms