Córdoba, Argentina – Un operativo policial inusual se desplegó este martes en el barrio Yofre Norte de la ciudad de Córdoba, tras el descubrimiento de un proyectil de mortero abandonado junto a un contenedor de residuos. El hallazgo, reportado alrededor de las 3:50 p.m. Por un vecino a través del número de emergencias 911, desencadenó una rápida respuesta de las autoridades y la evacuación preventiva de la zona, convirtiéndose en un evento que los residentes describieron como “de película”.
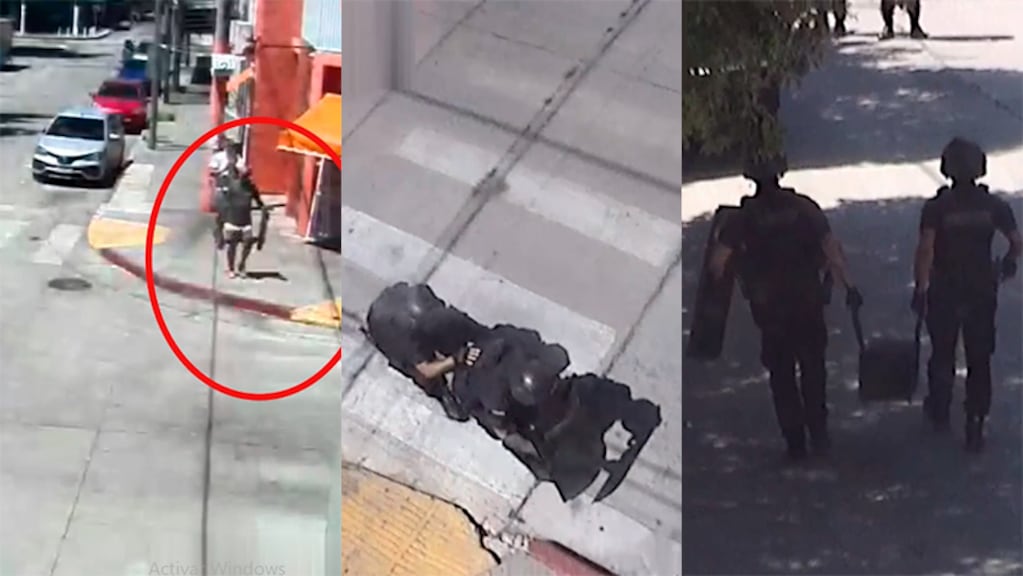
La situación rápidamente escaló con la intervención del programa Cordobeses en Alerta y, posteriormente, de la Brigada de Explosivos de la Policía de Córdoba. Especialistas aseguraron el perímetro alrededor de la calle Jacinto de Altolaguirre al 2100, donde se encontró el artefacto, y procedieron a la remoción controlada del mismo. La presencia del explosivo generó preocupación entre los vecinos, quienes observaron el operativo con atención.
Detalles del Artefacto y el Operativo
Tras ser trasladado a la base operativa para su análisis, los peritos confirmaron que el objeto era un proyectil de mortero de 120 milímetros, de origen bélico. Afortunadamente, el proyectil se encontraba en mal estado de conservación y sin capacidad de activación al momento del hallazgo, minimizando el riesgo para la población. El operativo policial se desarrolló sin incidentes, y no se reportaron heridos ni daños materiales, según informes oficiales. Jacinto de Altolaguirre, una calle principal en el barrio Yofre Norte, fue el centro de la actividad policial, interrumpiendo el tráfico y la rutina diaria de los residentes. NuestraCiudad describe la calle como una importante vía comercial en la zona.
El Centro Vecinal Yofre Norte, ubicado también en Jacinto de Altolaguirre, se encuentra cerca del área donde se encontró el explosivo, según Mapcarta. La rápida respuesta de las autoridades y la evacuación preventiva fueron cruciales para garantizar la seguridad de los vecinos.
Investigación en Curso
Las autoridades judiciales han iniciado una investigación para determinar cómo el proyectil de mortero terminó abandonado en un contenedor de basura en una zona residencial. La presencia de un artefacto explosivo de este tipo en un área urbana plantea interrogantes sobre su origen y cómo llegó a estar allí. La investigación busca esclarecer las circunstancias del hallazgo y determinar si hubo alguna negligencia o actividad ilegal involucrada.
Este incidente se produce en un contexto de creciente preocupación por la seguridad pública en la ciudad de Córdoba. Aunque el proyectil no representaba una amenaza inmediata, su descubrimiento subraya la importancia de la vigilancia y la rápida respuesta ante situaciones de riesgo. La policía continúa trabajando para garantizar la seguridad de los ciudadanos y prevenir incidentes similares en el futuro.
Mientras tanto, la comunidad de Yofre Norte intenta volver a la normalidad tras el operativo. El incidente ha generado debate sobre la necesidad de reforzar las medidas de seguridad y la importancia de la colaboración ciudadana en la prevención de delitos. La Justicia espera obtener más información a medida que avanza la investigación.
La rápida acción de los vecinos al alertar a las autoridades y la eficiente respuesta de la Brigada de Explosivos fueron fundamentales para evitar cualquier daño a personas o propiedades. Este caso sirve como un recordatorio de la importancia de la comunicación y la coordinación entre la comunidad y las fuerzas de seguridad.
¿Qué medidas adicionales podrían implementarse para prevenir la presencia de artefactos peligrosos en áreas residenciales? La investigación en curso podría arrojar luz sobre este asunto y conducir a la adopción de nuevas políticas de seguridad.
A medida que la investigación avanza, se espera que se revelen más detalles sobre el origen del proyectil y las circunstancias que llevaron a su abandono. La comunidad de Yofre Norte permanece atenta a los avances del caso y espera que se tomen las medidas necesarias para garantizar su seguridad.
Comparte tus pensamientos sobre este inusual operativo en los comentarios a continuación.