The $10 Million Baby: How Personalized Gene Editing is Redefining Medicine – and What It Means for You
The cost of fixing a single genetic defect in a newborn can easily exceed the price of a luxury mansion. That startling reality, highlighted by the recent success in treating a rare liver disease, isn’t a medical anomaly – it’s a glimpse into the future of medicine. The FDA is now actively charting a course for approving these personalized gene-editing treatments, moving beyond the realm of experimental therapies and towards a new era of precision healthcare. But this revolution won’t be cheap, and its benefits won’t be evenly distributed.
A Landmark Case: KJ’s Journey and the Challenges of ‘N=1’
Six months ago, the medical community celebrated the successful treatment of “KJ,” an infant born with a uniquely devastating genetic liver disease. Researchers painstakingly crafted a custom CRISPR-based therapy to correct the specific mutation causing KJ’s illness. This achievement, detailed in the New England Journal of Medicine, was a triumph of scientific collaboration. However, it also underscored a critical challenge: the current model for gene therapy is largely unsustainable for widespread application. The process required a massive, coordinated effort from dozens of scientists, often working without traditional funding structures. The exact cost remains undisclosed, but estimates range into the tens of millions of dollars – a figure that raises profound questions about accessibility and equity.
The FDA’s Roadmap: Navigating the Complexities of Personalized Therapies
The FDA’s recently unveiled roadmap focuses on establishing clear regulatory pathways for these highly individualized treatments. A key component is the development of robust methods for assessing the safety and efficacy of therapies designed for a single patient, or a very small cohort. Traditional clinical trials, designed for broadly applicable drugs, are ill-suited for this purpose. The FDA is exploring innovative approaches, including real-world evidence and adaptive trial designs, to overcome these hurdles. This includes a greater emphasis on accelerated approval pathways for life-threatening conditions where no alternative treatments exist.
Beyond CRISPR: The Expanding Toolkit of Gene Editing
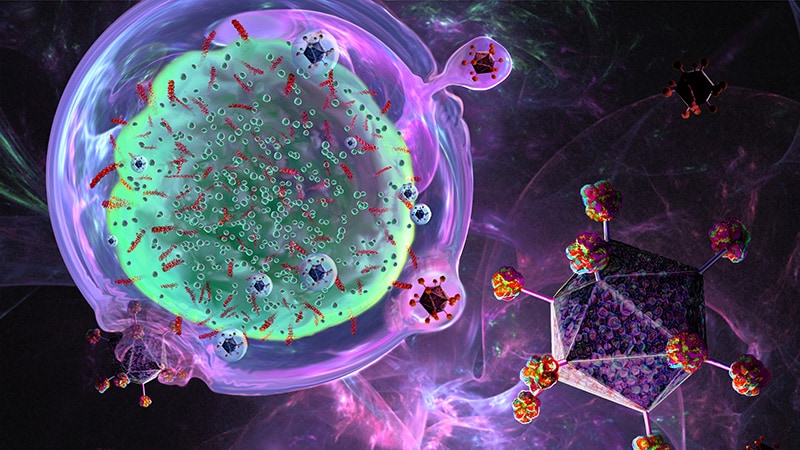
While CRISPR-Cas9 has dominated the headlines, the field of gene editing technologies is rapidly evolving. Base editing, prime editing, and other emerging techniques offer greater precision and reduced off-target effects. These advancements are crucial for minimizing the risks associated with altering the human genome. Furthermore, the development of more efficient delivery systems – such as adeno-associated viruses (AAVs) and lipid nanoparticles – is essential for reaching the affected tissues and cells. The convergence of these technologies promises to unlock even more personalized and effective therapies.
The Cost Conundrum: Making Gene Editing Accessible
The exorbitant cost of personalized gene editing remains the biggest barrier to widespread adoption. Several strategies are being explored to address this challenge. These include: reducing manufacturing costs through process optimization, developing more efficient gene editing tools, and exploring innovative financing models, such as outcome-based pricing and public-private partnerships. The potential for genomic medicine to transform healthcare is immense, but only if it can be made accessible to those who need it most. The current system, reliant on bespoke solutions, is simply not scalable.
The Future of Personalized Medicine: From Rare Diseases to Common Conditions?
Initially, personalized gene editing will likely remain focused on ultra-rare genetic diseases, where the unmet medical need is greatest and the regulatory pathway is more streamlined. However, the long-term vision extends far beyond these niche applications. Researchers are already investigating the potential of gene editing to treat common conditions, such as cancer, heart disease, and Alzheimer’s disease. The ability to tailor therapies to an individual’s unique genetic profile could revolutionize the way we prevent and treat illness. The rise of sophisticated genomic sequencing and data analytics will be critical to realizing this potential. Expect to see a growing demand for skilled professionals in genetics and genomics as this field expands.
The journey from the “$10 million baby” to affordable, accessible gene editing is a long one. But the FDA’s roadmap signals a clear commitment to navigating the complexities and unlocking the transformative power of personalized medicine. What are your predictions for the future of gene editing and its impact on healthcare? Share your thoughts in the comments below!