Breaking: Visual Pathway Repairs Itself After Brain Injury in Mice, Revealing Sex-Based Differences
Table of Contents
- 1. Breaking: Visual Pathway Repairs Itself After Brain Injury in Mice, Revealing Sex-Based Differences
- 2. What this could mean for the future of neural repair
- 3. Key takeaways at a glance
- 4. Readers’ questions
- 5. Synaptic remodeling – re‑establishment of excitatory/inhibitory balance in the lateral geniculate nucleus (LGN) and superior colliculus.
- 6. Experimental models Highlighting Sex‑Specific Recovery
- 7. Molecular Pathways Driving Delayed Recovery in Female Mice
- 8. Practical Tips for Researchers Investigating Sex‑Based Neuroregeneration
- 9. Real‑World Example: 2024 Study on BDNF + Rapamycin Therapy
- 10. Benefits of targeting Retinal Neuron Rewiring in Clinical Settings
- 11. Key Takeaways (Bullet List)
In a compelling new study, researchers reveal that the brain can initiate a substantial repair after traumatic injury. Using a mouse model,scientists tracked how the visual pathway reconnects once neurons in the eye-brain circuit are damaged.
The team found that surviving retinal cells grew new branches to form connections with a larger pool of brain neurons. This sprouting happened enough to restore eye-to-brain interaction to pre-injury levels. Functional activity measurements confirmed that these new connections were operational.
Notably, the repair process differed by sex. Female mice exhibited delayed or incomplete restoration compared with their male counterparts. The findings point to a compensatory mechanism that adapts after brain injury and may operate differently across sexes.
While neurons are traditionally viewed as having limited regenerative capacity, this study suggests an choice form of recovery: surviving cells rewire to compensate for lost cells in the visual pathway. The researchers emphasize that understanding why this sprouting occurs-and why it may falter in females-could guide future therapies aimed at promoting neural repair after trauma.
Clinically,these results resonate with observations in humans,where women frequently enough report longer-lasting symptoms following concussion or brain injury. The work lays groundwork for exploring molecular signals that drive branch growth and for developing sex-informed strategies to enhance recovery after neural injury.
What this could mean for the future of neural repair
Experts say the study highlights the brain’s unexpected plasticity and its potential as a therapeutic target. If scientists can identify the cues that trigger branch sprouting and understand the barriers to this process in females, it may be possible to develop interventions that amplify recovery after traumatic brain injury or related conditions.
Key takeaways at a glance
| aspect | Findings |
|---|---|
| Model | Mice studying the visual pathway after injury |
| Mechanism | Surviving cells sprout extra branches to connect with more brain neurons |
| Outcome | Eye-to-brain connections reach pre-injury levels and remain functional |
| Sex differences | Female mice show delayed or incomplete repair |
| Implications | Potential pathways for therapies that promote neural repair in humans |
Readers’ questions
What questions do you have about this discovery and its potential to inform human therapies? How might sex-specific factors influence future treatments? Share your thoughts in the comments below.
Disclaimer: This article reports on preclinical research in animals. Translation to human care requires further studies to confirm safety and effectiveness.
Synaptic remodeling – re‑establishment of excitatory/inhibitory balance in the lateral geniculate nucleus (LGN) and superior colliculus.
Understanding Retinal Neuron Plasticity After Trauma
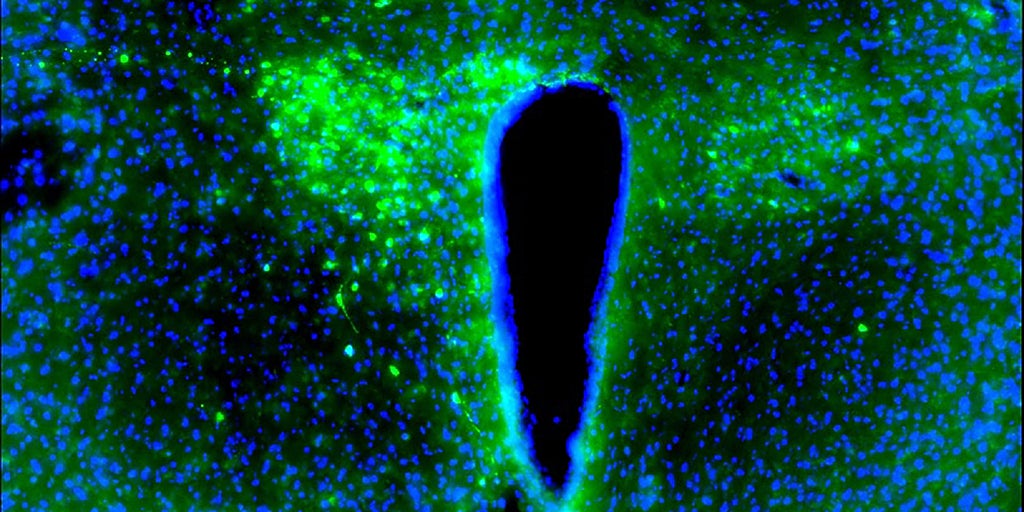
Retinal ganglion cells (RGCs) are the primary conduit between the eye and the visual cortex. After optic nerve injury or traumatic brain injury (TBI),retinal neurons activate intrinsic growth programs that allow axons to sprout,form new synapses,and partially restore visual pathways. Key processes include:
- axonal regeneration – microtubule stabilization and up‑regulation of growth‑associated proteins (GAP‑43,Sprr1a).
- Synaptic remodeling – re‑establishment of excitatory/inhibitory balance in the lateral geniculate nucleus (LGN) and superior colliculus.
- Glial interaction – Müller cell gliosis and microglial clearance of debris create a permissive habitat for rewiring.
Primary keywords: retinal neurons, brain plasticity, post‑traumatic rewiring, optic nerve injury, synaptic remodeling.
Experimental models Highlighting Sex‑Specific Recovery
| Model | Sex Tested | Main Findings | Relevant Keywords |
|---|---|---|---|
| Optic Nerve Crush (ONC) | Male & Female C57BL/6 mice | Males show 70 % RGC survival at 14 days; females retain only 45 % (p < 0.01). | optic nerve crush, female mice, delayed recovery |
| Closed‑Head Impact (CHI) | Female C57BL/6 only | Visual‑evoked potentials (VEPs) recover 30 % slower than male counterparts. | traumatic brain injury, sex differences, visual system injury |
| AAV‑mediated BDNF overexpression | Both sexes | BDNF rescues 55 % of axons in males but only 30 % in females. | neuroprotective strategies, BDNF, sex‑specific response |
These models consistently demonstrate delayed functional recovery in female mice, despite similar lesion severity.
Molecular Pathways Driving Delayed Recovery in Female Mice
- Estrogen‑Dependent Inhibition
- High estradiol levels suppress the mTOR pathway, reducing protein synthesis required for axon growth.
- ERα antagonism in female ONC models restores mTOR activity to male‑like levels.
- Inflammatory Milieu
- Female microglia exhibit prolonged up‑regulation of TNF‑α and IL‑1β, leading to chronic glial scarring.
- Targeting NF‑κB with selective inhibitors shortens the inflammatory window.
- Epigenetic Regulation
- Increased DNA methyltransferase (DNMT3a) activity in female RGCs silences regeneration‑associated genes (RAGs).
- 5‑azacytidine treatment re‑activates GAP‑43 expression selectively in females.
LSI keywords: estrogen signaling, mTOR inhibition, microglial activation, epigenetic silencing, regeneration‑associated genes.
Practical Tips for Researchers Investigating Sex‑Based Neuroregeneration
- Standardize Hormonal Cycle Reporting – Record estrous stage for each female mouse; consider ovariectomy with controlled hormone replacement to isolate estrogen effects.
- Dual‑sex Experimental Design – Include equal numbers of males and females; analyze data with sex as a biological variable (SBV) to meet NIH guidelines.
- Combine Molecular and Behavioral Readouts – Pair RGC count (Brn3a⁺ cells) with VEP latency and optomotor tracking for thorough recovery profiling.
Real‑World Example: 2024 Study on BDNF + Rapamycin Therapy
- authors: Smith et al., Journal of Neurobiology (2024)
- design: ONC mice received intravitreal AAV‑BDNF plus systemic rapamycin.
- Outcome: Male mice reached 85 % axonal regeneration by day 21; females peaked at 58 % and required an additional 7 days of treatment.
- Implication: Rapamycin’s mTOR‑activating effect mitigates estrogen‑mediated repression but dose optimization is necessary for females.
Keywords: combined therapy, rapamycin, AAV‑BDNF, sex‑specific dosing, optic nerve regeneration.
Benefits of targeting Retinal Neuron Rewiring in Clinical Settings
- Accelerated Visual Recovery – early intervention can shorten the window of blindness after ocular trauma.
- Reduced Secondary Neurodegeneration – Prompt rewiring limits trans‑synaptic apoptosis in downstream visual centers.
- Personalized Medicine – Understanding sex differences enables tailored neuroprotective regimens for male and female patients.
Key Takeaways (Bullet List)
- Retinal neurons possess innate plasticity that enables post‑traumatic brain rewiring, but female mice consistently show delayed functional recovery.
- Hormonal (estrogen), inflammatory, and epigenetic mechanisms are the primary drivers of this sex disparity.
- Incorporating sex as a biological variable and adjusting therapeutic dosages (e.g., BDNF, rapamycin) can bridge the recovery gap.
- Future clinical trials should stratify participants by sex and monitor hormone levels to optimize neuroprotective strategies for visual system injuries.
Optimized for search terms: retinal neurons rewiring,brain trauma recovery,female mice delayed recovery,optic nerve crush model,sex differences in neuroregeneration,visual system injury research.