Lung Cancer’s Silent Shift: Why Non-Smokers Are Increasingly at Risk – and What You Need to Know
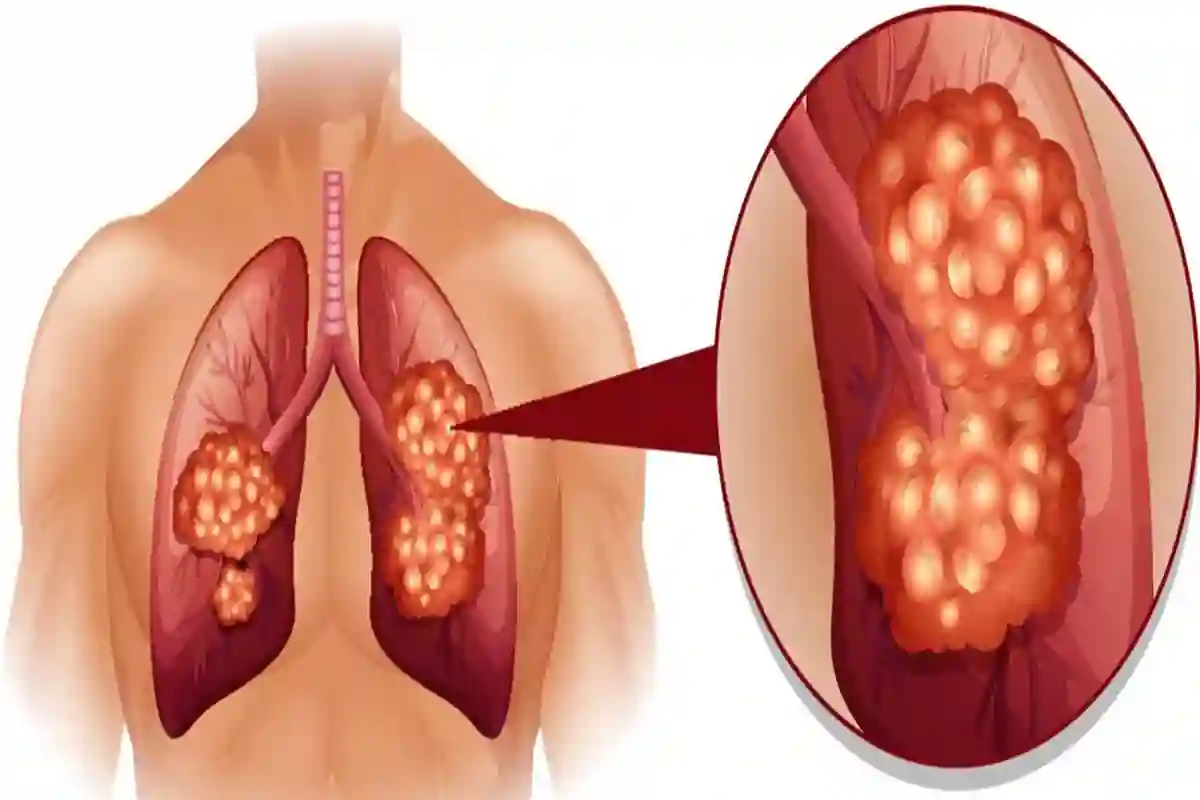
Imagine a future where the primary threat of lung cancer isn’t tied to decades of smoking, but to the very air we breathe. This isn’t science fiction; it’s a rapidly evolving reality. While lung cancer remains a formidable challenge – with 64% survival rates for early detection plummeting to just 8% in advanced stages, according to the National Institutes of Health – a concerning trend is emerging: a significant rise in diagnoses among individuals who have never smoked. This shift demands a re-evaluation of risk factors, prevention strategies, and early detection methods.
The Rising Tide of Non-Smoker Lung Cancer
Across India, and globally, oncologists are witnessing a disturbing increase in lung cancer cases among non-smokers. Dr. Satheesh CT, senior consultant, medical oncology at HCG Cancer Hospitals, Bengaluru, cautions, “Lung cancer is no longer a smoker’s disease.” This isn’t simply a statistical anomaly; it reflects a fundamental change in the environmental and lifestyle factors contributing to the disease. Approximately 25-40% of lung cancer cases in India now occur in non-smokers, a figure that’s steadily climbing.
But what’s driving this change? The answer, experts say, is multifaceted. It’s a confluence of escalating air pollution, increased exposure to second-hand smoke, and, importantly, genetic predispositions.
The Invisible Threat: Air Pollution and PM2.5
Air pollution, particularly the presence of fine particulate matter (PM2.5), is a major culprit. These microscopic particles can penetrate deep into the lungs and even enter the bloodstream, delivering carcinogenic substances directly to organs. “The PM2.5 has the tendency to enter our bloodstream, making our organs exposed and vulnerable to carcinogens,” explains Dr. Satheesh. This is particularly concerning in urban areas and regions with high levels of industrial activity.
Lung cancer isn’t solely an outdoor issue. Indoor air quality plays a crucial role. Kitchen smoke, often underestimated, is a significant source of pollutants, especially for homemakers. Exposure to second-hand smoke, even intermittent, dramatically increases risk for non-smokers.
Recognizing the Subtle Signs: Early Detection is Key
Early detection remains the most powerful weapon against lung cancer, but the symptoms can be subtle, especially in non-smokers. While smokers may experience coughing up blood, wheezing, and recurring infections, non-smokers often present with more ambiguous symptoms.
Dr. Satheesh highlights key warning signs to watch for:
- Persistent dry cough
- Breathlessness on exertion
- Unexplained fatigue
- Chest discomfort
- Weight loss
“As a caregiver, if such symptoms persist beyond a usual cold/flu, especially in someone exposed to pollution or indoor smoke, seek a specialist opinion,” Dr. Satheesh advises. Don’t dismiss these symptoms as simply being “stressed” or “out of shape.”
The Future of Lung Cancer Treatment: Personalized Medicine
The good news is that advancements in treatment are offering new hope, particularly for non-smokers. Targeted therapies, designed to address specific genetic mutations within cancer cells, are proving increasingly effective.
Genetic testing is becoming increasingly crucial in tailoring treatment plans. Identifying mutations like EGFR and ALK allows oncologists to select therapies that specifically target these vulnerabilities, maximizing effectiveness and minimizing side effects. This move towards personalized medicine represents a significant leap forward in lung cancer care.
The Role of Liquid Biopsies
Beyond traditional tissue biopsies, liquid biopsies – analyzing circulating tumor DNA in the bloodstream – are emerging as a promising tool for early detection, monitoring treatment response, and identifying genetic mutations without invasive procedures. While still evolving, liquid biopsies hold the potential to revolutionize lung cancer management.
Protecting Your Lungs: Proactive Steps for a Healthier Future
While genetic predisposition can’t be altered, proactive steps can significantly reduce your risk. Prevention is paramount.
- Improve Indoor Air Quality: Ensure good kitchen ventilation and adopt safer cooking habits.
- Limit Pollution Exposure: Reduce outdoor activities during peak pollution times and wear a high-quality mask when necessary.
- Maintain a Smoke-Free Home: Protect yourself and your family from the dangers of second-hand smoke.
- Prioritize Lung Health: Regular check-ups, a healthy diet rich in antioxidants, and regular physical activity are essential.
See our guide on improving indoor air quality for more detailed tips.
The Rise of Air Purification Technology
The demand for effective air purification solutions is surging. Advanced air purifiers equipped with HEPA filters and activated carbon can remove PM2.5 and other harmful pollutants from indoor air. However, it’s crucial to choose a purifier that’s appropriately sized for the room and regularly maintain the filters for optimal performance.
Frequently Asked Questions
Q: Is lung cancer only a concern for smokers?
A: No. While smoking remains a major risk factor, a growing number of non-smokers are being diagnosed with lung cancer due to factors like air pollution, second-hand smoke, and genetic predisposition.
Q: What are the early symptoms of lung cancer in non-smokers?
A: Common symptoms include a persistent dry cough, breathlessness, unexplained fatigue, chest discomfort, and weight loss.
Q: What is targeted therapy and how does it help?
A: Targeted therapy focuses on specific genetic mutations within cancer cells, allowing for more precise and effective treatment with fewer side effects.
Q: Can I reduce my risk of lung cancer even if I have a genetic predisposition?
A: Yes. Reducing exposure to pollutants, maintaining a healthy lifestyle, and undergoing regular check-ups can significantly lower your risk.
Lung cancer in India is undergoing a quiet revolution. It’s no longer solely a smoker’s disease, but a public health challenge demanding awareness, proactive prevention, and continued research. The air we breathe, the choices we make, and the speed with which we respond to early warning signs will collectively shape the future of lung health. What small, mindful actions will you take today to protect your lungs?