Rapid salmonella Detection: New Strategy Promises Same-Day Results, Protecting consumers
A groundbreaking new detection strategy offers a fast, low-cost solution for identifying Salmonella in food – possibly preventing contaminated products from reaching consumers. A study published in Frontiers in Microbiology details a Real-time PCR-based method capable of detecting Salmonella in meats, vegetables, and dairy within just seven hours, a notable leap forward from the traditional five-day process.
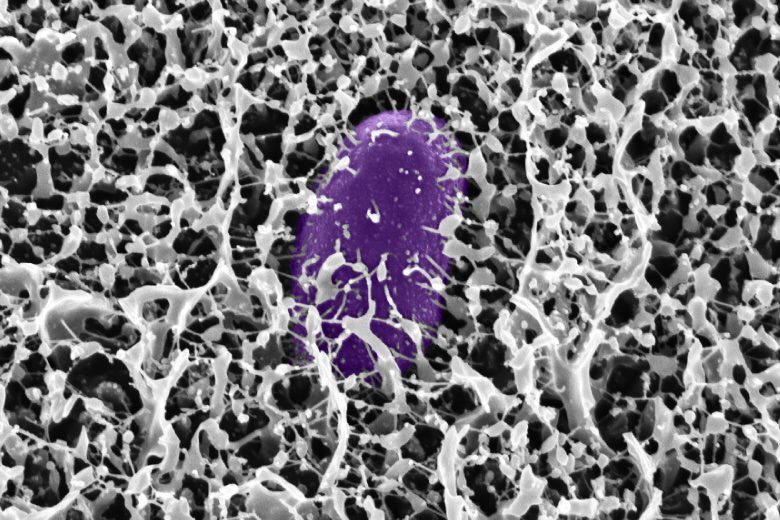
(Image: New rapid PCR method detects Salmonella in food within hours – Microgen / Shutterstock.com)
The Threat of Salmonella
Salmonella is a major global health concern, responsible for over half of all foodborne illnesses worldwide.The infection causes an estimated hundreds of thousands of deaths annually, with approximately 18 infections per 100,000 people in Europe alone.Two primary Salmonella species, Salmonella enterica and All the Balmonics, encompass over 2,600 serotypes capable of infecting both animals and humans.
common sources of infection include contaminated meat, eggs, and contact with infected animals. Though, Salmonella can also be found in pig meat, bakery items, dairy products, and vegetables.
Current Detection Methods: A Time-Consuming Process
Currently, Salmonella isolation relies on lengthy analytical reference methods. These methods,while reliable,require a pre-enrichment period allowing the pathogen to grow – a process that takes at least five days to yield results.
In the event of an outbreak, this delay can hinder efforts to quickly identify the source of contamination and prevent further spread. While PCR diagnostics have emerged as faster alternatives, many are technically complex and still time-consuming.
A New Approach: Rapid, Cost-Effective PCR
Researchers have developed a highly versatile, qualitative real-time PCR method for rapid Salmonella detection across diverse food matrices. The study focused on evaluating various combinations of DNA extraction methods,enrichment broths,and incubation conditions to optimize the