Discover the latest in health: evidence‑based wellness tips, medical breakthroughs, nutrition guidance, fitness insights, and expert advice for a healthier, happier life.
Alzheimer’s Breakthrough? Scientists Re-Evaluate TREM2‘s Role After Trial Setback
Table of Contents
- 1. Alzheimer’s Breakthrough? Scientists Re-Evaluate TREM2’s Role After Trial Setback
- 2. INVOKE-2 Trial Results Prompt Rethinking
- 3. What Does This Mean for Future Research?
- 4. Understanding TREM2: An Evergreen Viewpoint
- 5. Alternative Approaches to Alzheimer’s Treatment
- 6. The Everlasting quest for Alzheimer’s Solutions
- 7. Frequently Asked Questions About Alzheimer’s Research
- 8. Here’s a PAA-related question, tailored to the provided content:
- 9. TREM2 & Alzheimer’s: Unpacking the implications of the INVOKE-2 Trial
- 10. Understanding TREM2 and its Role in Alzheimer’s Disease
- 11. TREM2 and Amyloid Plaques
- 12. The INVOKE-2 Trial: A Closer look
- 13. Future Directions for TREM2-Based Therapies in Alzheimer’s
- 14. Frequently Asked Questions (FAQ) about TREM2 and alzheimer’s
The Fight Against Alzheimer’s Disease Has Taken An Unexpected Turn. Following the disappointing results from the INVOKE-2 trial, scientists are critically re-evaluating the role of TREM2 as a therapeutic target for this devastating neurodegenerative condition.
Published Online Today, July 2, 2025, the study highlights the complexities of Alzheimer’s and the need for diversified research strategies.The initial hope was that targeting TREM2,a protein involved in immune response in the brain,could offer a novel way to combat the disease.
INVOKE-2 Trial Results Prompt Rethinking
The INVOKE-2 trial, designed to assess the efficacy of a TREM2-activating drug, failed to meet its primary endpoints. This surprising outcome has urged experts worldwide to reconsider the prevailing hypotheses surrounding TREM2’s function in Alzheimer’s pathology.
The Focus Is Now Shifting towards understanding why the intervention didn’t yield the anticipated benefits and exploring alternative therapeutic approaches. The unexpected results emphasize the intricate nature of Alzheimer’s and the challenges in developing effective treatments.
What Does This Mean for Future Research?
The Failure of The INVOKE-2 trial doesn’t signify the end of Alzheimer’s research. Instead, it serves as a crucial learning opportunity. Researchers are actively exploring new avenues, including:
- investigating different stages of the disease where TREM2 intervention might be more effective.
- Focusing on combination therapies that address multiple aspects of Alzheimer’s pathology.
- exploring personalized medicine approaches tailored to individual genetic and biomarker profiles.
This re-evaluation could lead to more targeted and effective strategies in the long run, moving the field closer to meaningful treatments and preventative measures.
Understanding TREM2: An Evergreen Viewpoint
Even though the INVOKE-2 trial had setbacks,understanding the role of TREM2 remains crucial.
TREM2 Functions Primarily As An Immune Receptor found on Microglia, the brain’s resident immune cells. It plays a crucial role in clearing cellular debris and amyloid plaques, hallmarks of Alzheimer’s disease.
Did You Know? Genetic variations in TREM2 have been linked to an increased risk of developing Alzheimer’s, highlighting its significance in the disease process.
Despite the recent trial outcome, ongoing research continues to investigate the intricacies of TREM2 and its potential as a therapeutic target.
Alternative Approaches to Alzheimer’s Treatment
While Researchers Re-Assess The TREM2 Strategy, other promising avenues are being pursued:
- Targeting Amyloid Plaques: Drugs like Lecanemab have shown promise in removing amyloid plaques from the brain.
- Addressing Tau Tangles: Scientists are developing therapies to prevent the formation and spread of tau tangles, another key feature of Alzheimer’s.
- Lifestyle Interventions: Studies suggest that diet,exercise,and cognitive stimulation can help reduce the risk of cognitive decline.
The Future Of Alzheimer’s Treatment likely involves a multi-faceted approach that combines pharmacological interventions with lifestyle modifications.
| approach | Target | Status |
|---|---|---|
| TREM2 Modulation | Immune Response | Under Re-evaluation |
| Amyloid Plaque Removal | Amyloid Plaques | Approved Therapies Available |
| Tau Tangle Inhibition | Tau Tangles | Ongoing Research |
The Everlasting quest for Alzheimer’s Solutions
Alzheimer’s Disease Remains One of The Greatest Health Challenges of our time. The global search for effective treatments continues relentlessly,fueled by dedication and technological advancements.
Recent advancements in neuroimaging, biomarker revelation, and genetics are providing valuable insights into the disease’s underlying mechanisms.This knowledge is crucial for developing more targeted and effective interventions.
The hope is that continued efforts will ultimately lead to breakthroughs that can prevent,delay,or even reverse the course of Alzheimer’s disease.
Pro Tip: Early diagnosis and intervention are crucial for managing Alzheimer’s symptoms and maximizing quality of life. If you have concerns about memory loss or cognitive decline, consult a healthcare professional.
What other innovative approaches do you think hold promise for Alzheimer’s treatment?
Frequently Asked Questions About Alzheimer’s Research
- Why is the role of TREM2 being re-evaluated in Alzheimer’s research? Due to the INVOKE-2 trial failing, the role of TREM2 is being re-evaluated.
- What does the INVOKE-2 trial failure signify for Alzheimer’s research? The INVOKE-2 trial failure suggests that targeting TREM2 may not be as effective as initially hoped for.
- What are other potential targets being explored for Alzheimer’s treatment? Other potential targets include amyloid plaques, tau tangles, and inflammation pathways.
- How can I stay updated on the latest Alzheimer’s research? Follow reputable news sources, medical journals, and organizations dedicated to Alzheimer’s research.
- What are the symptoms of Alzheimer’s disease? Symptoms include memory loss, difficulty with problem-solving, and confusion.
- Is there a cure for Alzheimer’s? Currently, there is no cure for Alzheimer’s disease, but treatments help manage symptoms.
What are your thoughts on this re-evaluation of TREM2’s role? Share your comments below!
TREM2 & Alzheimer’s: Unpacking the implications of the INVOKE-2 Trial
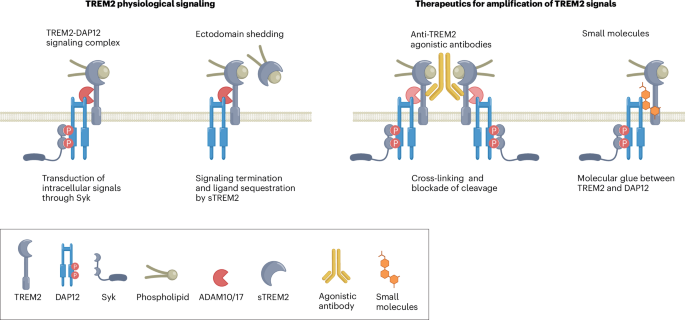
The landscape of Alzheimer’s disease (AD) research is constantly evolving, with researchers tirelessly working to develop effective treatments. One promising avenue of inquiry has been the role of the Triggering Receptor Expressed on Myeloid cells 2 (TREM2) protein. This article will explore the importance of TREM2 in AD, with a specific focus on the INVOKE-2 trial and its implications for the future of TREM2-targeted therapies.
Understanding TREM2 and its Role in Alzheimer’s Disease
TREM2 is a receptor primarily expressed on microglia, the brain’s resident immune cells. Its primary function is to recognize and respond to cellular debris and other signals within the brain. In the context of AD pathogenesis, TREM2 plays a crucial role in:
- Microglia Activation: TREM2 helps activate microglia, prompting them to engulf and clear amyloid plaques and other harmful materials.
- Inflammation Modulation: It can definitely help regulate the inflammatory response within the brain, possibly reducing neuroinflammation that contributes to AD progression.
- Neuronal Health: TREM2 signaling is implicated in supporting neuronal survival and function.
TREM2 and Amyloid Plaques
The accumulation of amyloid plaques is a hallmark of Alzheimer’s disease. TREM2 facilitates the microglia’s ability to clear these plaques, slowing down the disease’s progression. Defective TREM2 function is associated with increased amyloid plaque burden and an earlier age of Alzheimer’s onset. The complex interactions between TREM2, microglia, and amyloid plaques are the focus of much of the current research.
The INVOKE-2 Trial: A Closer look
The INVOKE-2 trial, a clinical study aiming to assess the efficacy of a TREM2-based therapy, has generated significant interest and anticipation in the Alzheimer’s research community. While the specific drug or treatment used in the trial is not detailed by the provided search results, the results of this trial are critically important for shaping the future of TREM2-targeted treatments. According to the provided search result, the INVOKE-2 results were disappointing.
The potential reasons for the trial’s outcome could be multifaceted and require careful consideration of various factors, including:
- Patient Population: The selection of participants may influence the therapy’s effectiveness.
- Dosage and Timing: The dosage of the therapy and the timing may not align with the optimal intervention window.
- Biomarker Impact: The impact on biomarkers, such as amyloid plaques or tau tangles, needs scrutiny.
- Target Specificity: the therapy’s mechanism and specificity for TREM2 might be incomplete.
Further analysis of the data, including subgroup analyses for specific populations, may provide a clearer understanding of the results.
Future Directions for TREM2-Based Therapies in Alzheimer’s
The INVOKE-2 trial outcomes, despite being disappointing, don’t mark the end of TREM2 research. Rather, the results inform future research and approaches by helping to refine future clinical trials. Several areas of research remain active, including:
- Improving Drug Progress: Researchers are developing more effective TREM2 activators.
- Patient selection: Better identification of patients most likely to benefit.
- Combination Therapies: Exploring TREM2-based treatments with other AD therapies.
- Advanced Imaging: Further research using advanced imaging may offer better insights into the disease’s impact on the brain.
The development of complex treatments for Alzheimer’s disease requires complete understanding. the ongoing work to target TREM2 holds promise for the future of Alzheimer’s treatment, despite challenges. The progress of TREM2-targeted therapies underscores the complexity of the disease and the need for sustained research.
Frequently Asked Questions (FAQ) about TREM2 and alzheimer’s
Here are some frequently asked questions regarding TREM2 and its influence in Alzheimer’s disease:
What is TREM2?
TREM2 is a protein found on microglia, the immune cells of the brain. It is important for clearing debris, regulating inflammation, and possibly promoting neuron survival.
Why target TREM2 for Alzheimer’s?
By targeting TREM2, doctors hope to enhance microglia’s ability to clear amyloid plaques, control inflammation, and protect nerve cells. These steps may help slow or stop the progression of Alzheimer’s disease.
What was the outcome of the INVOKE-2 trial?
While the source doesn’t provide specific details, it notes that the INVOKE-2 trial results were disappointing; they may indicate challenges in TREM2-target therapy.
What are the future research directions for TREM2 based therapies?
Researchers are investigating better drug designs, targeting specific patient groups, developing combination therapies, and employing advanced imaging methods to better understand and use TREM2 in Alzheimer’s treatment.